EFFICACY OF ANESTHETIC COCKTAIL WOUND INSTILLATION FOR POSTOPERATIVE ANALGESIA FOLLOWING POSTERIOR SPINAL SURGERY
DOI:
https://doi.org/10.55374/jseamed.v4i2.71Keywords:
Posterior spinal surgery, Anesthetic cocktail, Postoperative pain, Wound instillationAbstract
Background: Posterior spinal surgery is a common procedure in orthopedic practices that causes severe pain after surgery. Proper postoperative pain controls not only benefit early mobilization and initiation of physiotherapy but they also play important roles in reducing morbidity and mortality.
Objective: This prospective, double-blinded, randomized controlled study investigated the efficacy of anesthetic cocktail wound instillation for postoperative analgesia following posterior spinal surgery.
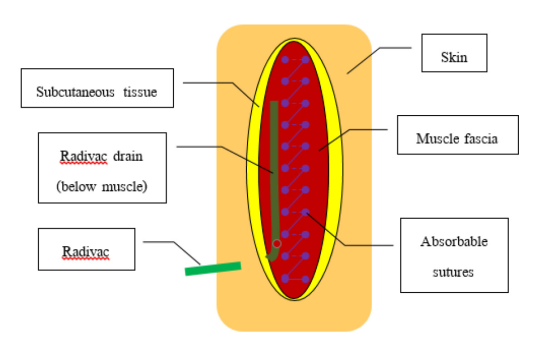
Methods: After posterior spinal surgery, 54 patients were randomized to instill 20 mL of normal saline (Group N) or anesthetic cocktail consisting bupivacaine, ketorolac and morphine (Group A) in the wound after securing hemostasis and leaving a contact time of 60 seconds. After a dwell time of 60 seconds, the wound layers were closed without mopping or suctioning. All patients in both groups received patient-controlled analgesia using morphine for 24 hours post surgery, followed by standard analgesia. The analgesia consumption (morphine), visual analog scale (VAS) at specific hours after the operation, and time for first demand of analgesia were recorded. Morphine-related side effects were also monitored.
Results: The patients in group A consumed significantly less morphine at 4, 8, 12 and 16 hours after the surgery (p=0.048, 0.007, 0.005 and 0.026, respectively). In addition, they had lower VAS over the first 24 hours (p<0.05) and longer median duration of first demand of analgesia (p=0.013). Morphinerelated side effects were also lower in group A (p=0.024). Conclusion: The simple technique of wound instillation with anesthetic cocktail significantly reduced postoperative requirements of morphine and improved pain control with lower rates of nausea and vomiting over the first postoperative day after posterior spinal surgery.
Downloads
Metrics
References
Jonnavithula N, Garre S, Pasupuleti S, Durga P, Kulkarni DK, Ramachandran G .Wound instillation of local anesthetic bupivacaine for postoperative analgesia following lumbar laminectomy. Middle East J Anaesthesiol 2015; 23: 193-8.
Bajwa SJ, Haldar R. Pain management following spinal surgeries: an appraisal of the available options. J Craniovertebr Junction Spine 2015; 6: 105-10. DOI: https://doi.org/10.4103/0974-8237.161589
Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after Anesthesiology surgery: A prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013; 118: 934–44. DOI: https://doi.org/10.1097/ALN.0b013e31828866b3
Phillips DM. JCAHO pain management standards are unveiled. Joint commission on accreditation of healthcare organizations. JAMA 2000; 284: 428-9. DOI: https://doi.org/10.1001/jama.284.4.423b
Eldor J. Postoperative wound analgesia. A renewed modality. J NYSORA 2009; 13: 11-9.
Sinatra RS, Torres J, Bustos AM. Pain management after major orthopaedic surgery: current strategies and new concepts. J Am Acad Orthop Surg 2002; 10: 117-29. DOI: https://doi.org/10.5435/00124635-200203000-00007
Kvolik S, Kristek J, Sakic K, Takac I, Gulam D. A wound infiltration as a method of postoperative analgesia. Periodicum Biologorum 2009; 111: 241-6.
Tammachote N, Kanitnate S, Manuwong S, Yakumpor T, Panichkul P. Is pain after TKA better with periarticular injection or intrathecal morphine? Clin Orthop Relat Res 2013; 471: 1992-9. DOI: https://doi.org/10.1007/s11999-013-2826-9
Schenk MR, Putzier M, Kugler B, Tohtz S, Voigt K, Schink T. Postoperative analgesia after major spine surgery: patient-controlled epidural analgesia versus patient-controlled intravenous analgesia. Anesth Analg 2006; 103: 1311-7. DOI: https://doi.org/10.1213/01.ane/0000247966.49492.72
Kluba T, Hofmann F, Bredanger S, Blumenstock G, Niemeyer T. Efficacy of post-operative analgesia after posteriorlumbar instrumented fusion for degenerative disc disease: a prospective randomized comparison of epidural catheter and intravenous administration of analgesics. Orthop Rev 2010; 2: 27-30. DOI: https://doi.org/10.4081/or.2010.e9
Tian P, Fu X, Li Z, Ma X. Comparison of patient-controlled epidural analgesia and patient-controlled intravenous analgesia after spinal fusion surgery: a meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 2015; 16: 388. DOI: https://doi.org/10.1186/s12891-015-0849-y
Bianconi M, Ferraro L, Traina GC, Zanoli G, Antonelli T, Guberti A, et al. Pharmacokinetics and efficacy of ropivacaine continuous wound instillation after joint replacement surgery. Br J Anaesth 2003; 91: 830-5. DOI: https://doi.org/10.1093/bja/aeg277
Bulut T, Yilmazlar A, Yavascaoglu B, Sarisozen B. The effect of local anaesthetic on post-operative pain with wound instillation via a catheter for paediatric orthopaedic extremity surgery. J Child Orthop 2011; 5: 179-85. DOI: https://doi.org/10.1007/s11832-011-0337-3
Yuenyongviwat V, Pornrattanamaneewong C, Chinachoti T, Chareancholvanich K. Periarticular injection with bupivacaine for postoperative pain control in total knee replacement: a prospective randomized double-blind controlled trial. Adv Orthop 2012; 2012: 107309. DOI: https://doi.org/10.1155/2012/107309
Bianconi M, Ferraro L, Ricci R, Zanoli G, Antonelli T, Giulia B, et al. The pharmacokinetics and efficacy of ropivacaine continuous wound instillation after spine fusion surgery. Anesth Analg 2004; 98: 166–72. DOI: https://doi.org/10.1213/01.ANE.0000093310.47375.44
Koh IJ, Chang CB, Seo ES, Kim SJ, Seong SC, Kim TK. Pain management by periarticular multimodal drug injection after anterior cruciate ligament reconstruction: a randomized, controlled study. Arthroscopy 2012; 28:649-57. DOI: https://doi.org/10.1016/j.arthro.2011.10.015
Jung WH, Takeuchi R, Chun CW, Lee JS, Ha JH, Kim JH, et al. Efficacy of periarticular multimodal drug injection after medial opening-wedge high tibial osteotomy: a randomized, controlled study. Arthroscopy 2014; 30:1261-8. DOI: https://doi.org/10.1016/j.arthro.2014.04.104
Koehler D, Marsh JL, Karam M, Fruehling C, Willey M. Efficacy of surgical-Site, multimodal drug injection following operative management of femoral fractures: A randomized controlled trial. J Bone Joint Surg Am 2017; 99: 512-9. DOI: https://doi.org/10.2106/JBJS.16.00733
Andersen LJ, Poulsen T, Krogh B, Nielsen T. Postoperative analgesia in total hip arthroplasty: a randomized double-blinded, placebo-controlled study on peroperative and postoperative ropivacaine, ketorolac, and adrenaline wound infiltration. Acta Orthop 2007; 78: 187-92. DOI: https://doi.org/10.1080/17453670710013663
Liu W, Cong R, Li X, Wu Y, Wu H. Reduced opioid consumption and improved early rehabilitation with local and intraarticular cocktail analgesic injection in total hip arthroplasty: a randomized controlled clinical trial. Pain Med 2011; 12: 387-93. DOI: https://doi.org/10.1111/j.1526-4637.2010.01043.x
Moucha CS, Weiser MC, Levin EJ. Current Strategies in Anesthesia and Analgesia for Total Knee Arthroplasty. J Am Acad Orthop Surg 2016; 24: 60-73. DOI: https://doi.org/10.5435/JAAOS-D-14-00259
Busch CA, Shore BJ, Bhandari R, Ganapathy S, MacDonald SJ, Bourne RB, et al, Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am 2006; 88: 959-63. DOI: https://doi.org/10.2106/JBJS.E.00344
Kelley TC, Adams MJ, Mulliken BD, Dalury DF. Efficacy of multimodal perioperative analgesia protocol with periarticular medication injection in total knee arthroplasty: a randomized, double-blinded study. J Arthroplasty 2013; 28: 1274-7. DOI: https://doi.org/10.1016/j.arth.2013.03.008
Spangehl MJ, Clarke HD, Hentz JG, Misra L, Blocher JL, Seamans DP. The Chitranjan Ranawat Award: Periarticular injections and femoral & sciatic blocks provide similar pain relief after TKA: a randomized clinical trial. Clin Orthop Relat Res 2015; 473: 45-53. DOI: https://doi.org/10.1007/s11999-014-3603-0
Ozyilmaz K, Ayoglu H, Okyay RD, Yurtlu S, Koksal B, Hanci V, et al. Postoperative analgesic effects of wound infiltration with tramadol and levobupivacaine in lumbar disk surgeries. J Neurosurg Anesthesiol 2012; 24: 331-5. DOI: https://doi.org/10.1097/ANA.0b013e3182611a1d
Gordon DB, Stevenson KK, Griffie J, Muchka S, Rapp C, Ford-Roberts K. Opioid equianalgesic calculations. J Palliat Med 1999; 2: 209-18. DOI: https://doi.org/10.1089/jpm.1999.2.209
Lacy CF. Drug information handbook. 21st ed. Ohio, United Stages: Lexi-Comp; 2012.
McEvoy GK. American hospital formulary service drug information. 2014 ed. Maryland, United Stages: American Society of HealthSystem Pharmacists; 2014.
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







