COMPARISON OF PERCUTANEOUS PEDICLE SCREW FIXATION AND PEDICAL SCREW FIXATION IN CONVENTIONAL INCISION IN THORACOLUMBAR FRACTURE
DOI:
https://doi.org/10.55374/jseamed.v5i2.92Keywords:
Thoracolumbar Fracture, Percutaneous pedicle screw fixation, Open pedicle screw fixationAbstract
Background: Originally, patients with unstable thoracolumbar spine fracture were treated using pedicle screw fixation, a conventional incision. However, the small incision percutaneous pedicle screw fixation (PPSF), a new device, has been recently introduced which could save surgery time, reduce blood loss and improve clinical recovery.
Objective: This study aimed to evaluate postoperative outcomes of the PPSF, compared with the open pedicle screw fixation (OPSF) in conventional incision among patients with thoracolumbar fracture.
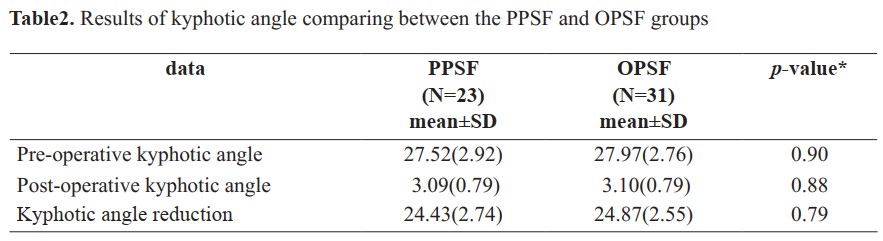
Methods: A retrospective study of 54 cases of patients with thoracolumbar spine fracture without neurological deficit was included in the study. The data were collected from medical records of patients admitted to Rayong Hospital from January 2017-December 2019. Results: Patients aged from 18-46 years (32.35+ 8.52) were mostly males (59.2%). Types of fracture included burst (72.22%). The most common level of thoracolumbar spine fracture was L1 (37.04%). Mostly, the cause of injury was fall from height (53.70%). The mean postoperative stays in the PPSF and OPSF groups were significant, 3.09±.59 and 6.16±1.003 days, respectively (p<0.05). The mean intraoperative blood losses of the PPSF and OPSF groups significantly differed, 44.35±15.02 and 466.13±87.92 mL, respectively (p < 0.01). However, the mean kyphotic angle reduction of the PPSF (24.43±2.74 degrees) and OPSF (24.87±2.55 degrees) groups did not significantly differ (p > 0.1). The mean postoperative pain score (VAS) at the first day in the PPSF and OPSF groups were 6.43±.94 and 6.61±.98, respectively, which did not significantly differ (p > 0.1).
Conclusion: PPSF spinal fracture treatment could reduce the amount of bleeding during surgery and reduce the length of hospital stay. However, the results of both types of surgery did not differ regarding postoperative pain, decreased kyphotic angle and surgical time.
Downloads
Metrics
References
Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine 1992; 17: 528-40. DOI: https://doi.org/10.1097/00007632-199205000-00010
Hasler RM, Exadaktylos AK. Bouamra O. Benneker LM, Clancy M, Sieber R, et al. Epidemiology and predictors of spinal injury in adult major trauma patients: European cohort study. Eur Spine J 2011; 20: 2174-80. DOI: https://doi.org/10.1007/s00586-011-1866-7
Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine 1983; 8: 817-31 DOI: https://doi.org/10.1097/00007632-198311000-00003
Vaccaro AR, Lehman RA Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine 2005; 30: 2325-33. DOI: https://doi.org/10.1097/01.brs.0000182986.43345.cb
Vaccaro AR, Zeiller SC, Hulbert RJ, Anderson PA, Harrin M, Hedlund R, et al. The thoracolumbar injury severity score: a proposed treatment algorithm. J Spinal Disord Tech 2005; 18: 209-15.
Lenarz CJ, Place HM. Evaluation of a new spine classification system, does it accurately predict treatment? J Spinal Disord Tech 2010; 23: 192-6. DOI: https://doi.org/10.1097/BSD.0b013e31819e30c1
Cimatti M, Forcato S, Polli F, Miscusi M, Frati A, Raco A. Pure percutaneous pedicle screw fixation without arthrodesis of 32 thoracolumbar fractures: clinical and radiological outcome with 36-month follow-up. Eur Spine J 2013; 22 (Suppl 6): S925-32. DOI: https://doi.org/10.1007/s00586-013-3016-x
Kim DY, Lee SH, Chung SK, Lee HY. Comparison of multifidus muscle atrophy and trunk extensor muscle strength: percutaneous versus open pedicle screw fixation. Spine 2005; 30: 123-9. DOI: https://doi.org/10.1097/01.brs.0000148999.21492.53
McAnany SJ, Overley SC, Kim JS, Baird EO, Qureshi SA, Anderson PA. Open versus minimally invasive fixation techniques for thoracolumbar trauma: A meta-analysis. Global Spine J 2016; 6: 186-94. DOI: https://doi.org/10.1055/s-0035-1554777
Phan K, Rao PJ, Mobbs RJ. Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: Systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg 2015; 135: 85-92. DOI: https://doi.org/10.1016/j.clineuro.2015.05.016
Vanek P, Bradac O, Konopkova R, de Lacy P, Lacman J, Benes V. Treatment of thoracolumbar trauma by short-segment percutaneous tranpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg 2014; 20:150-6. DOI: https://doi.org/10.3171/2013.11.SPINE13479
Wang H, Zhou Y, Li C, Liu J, Xiang L. Comparison of open versus percutaneous pedicle screw fixation using the sextant system in the treatment of traumatic thoracolumbar fractures. Clin Spine Surg 2017; 30: E239-e46. DOI: https://doi.org/10.1097/BSD.0000000000000135
Wild MH, Glees M, Plieschnegger C, Wenda K. Five-year follow-up examination after purely minimally invasive posterior stabilization of thoracolumbar fractures: a comparison of minimally invasive percutaneously and conventionally open treated patients. Arch Orthop Trauma Surg 2007; 127: 335-43. DOI: https://doi.org/10.1007/s00402-006-0264-9
Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE. The paraspinal sacrospinalissplitting approach to the lumbar spine. J Bone Jt Surg 1968; 50: 919-26. DOI: https://doi.org/10.2106/00004623-196850050-00004
LeeJK, Jang JW,Kim TW, Kim SH, Moon SJ. Percutaneous short-segment pedicle screw placement without fusion in the treatment of thoracolumbar burst fractures: is it effective?: comparative study with open short-segment pedicle screw fixation with posterolateral fusion. Acta Neurochir 2013; 155: 2305-12. DOI: https://doi.org/10.1007/s00701-013-1859-x
Fitschen-Oestern s, Scheuerlein F, Weuster M, Klueter T, Menzdorf L, Varoga D. et al. Reduction and retention of thoracolumbar fractures by minimally invasive stabilization versus open posterior instrumentation. Injury 2015; 46 (Suppl 4): S63-70. DOI: https://doi.org/10.1016/S0020-1383(15)30020-6
Dong SH, Chen HN, Tian JW, Xia T, Wang L, Zhao QH, et al. Effects of minimally invasive percutaneous and trans-spatium intermuscular short-segment pedicle instrumentation on thoracolumbar mono-segmental vertebral fractures without neurological compromise, Orthop Traumatol Surg Res 2013; 99: 405-11. DOI: https://doi.org/10.1016/j.otsr.2012.12.020
Grossbach AJ, Dahdaleh NS, Abel TJ, Woods GD, Dlouhy BJ, Hitchon PW. Injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. J Neurosurg 2013; 35: E2. DOI: https://doi.org/10.3171/2013.6.FOCUS13176
Rahul PP, Joshi V, Pemecha C, Kumar P, Bisnoi UP, Singh O. Comparative study between short segment open versus percutaneous pedicle screw fixation with indirect decompression in management of acute burst fracture of thoracolumbar spine with minimal neurological deficit in adults. J Spine 2016; 05: 1-5. DOI: https://doi.org/10.4172/2165-7939.1000339
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.