ANALYZING THE EARLY CLINICAL AND IMAGING OUTCOMES OF STA-MCA BYPASS SURGERY VIA THREE-DIMENSIONAL VOLUMETRIC MEASUREMENT IN PATIENTS WITH INTRACRANIAL ATHEROSCLEROSIS
DOI:
https://doi.org/10.55374/jseamed.v9.241Keywords:
recurrent stroke, cerebral revascularization, STA-MCA bypass, intracranial atherosclerosis, 3D volumetric measurement, case seriesAbstract
Background: Intracranial atherosclerotic disease (ICAD) is a leading cause of ischemic stroke and remains associated with high morbidity and mortality. Although recent studies suggest that superficial temporal artery to middle cerebral artery (STA–MCA) bypass may benefit patients with hemodynamic compromise, its clinical efficacy remains a matter of controversy.
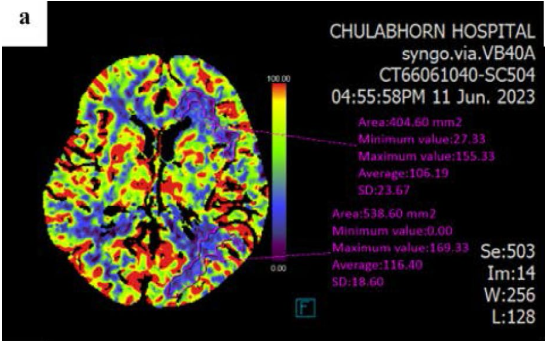
Objective: We aimed to evaluate the effectiveness of STA-MCA bypass surgery in patients with ICAD, focusing on both clinical outcomes and cerebral hemodynamic imaging using 3D volumetric analysis.
Methods: Six patients with ICAD who underwent STA-MCA bypass surgery were selected using predefined criteria. Clinical outcomes were retrospectively reviewed using the National Institutes of Health Stroke Scale (NIHSS) and the Modified Rankin Scale (mRS). Imaging outcomes were examined by analyzing the brain lesion area and perfusion using computed tomography perfusion (CTP). Statistical significance was analyzed using paired rank-sum and Friedman tests.
Results: In all cases, the primary diagnosis was ischemic stroke with significant stenosis of the internal carotid or middle cerebral artery. All patients demonstrated patent grafts, and no ischemic events occurred within 30 days after surgery. However, one patient had a postoperative asymptomatic acute subdural hematoma. All patients showed stable or improved neurological and functional outcomes after 30 days. Median NIHSS scores remained stable (pre-op 1.50 [0.00–7.50] vs. 30 days 1.50 [0.00–5.25], p = 0.368), while median mRS scores showed a non-significant trend toward improvement (pre-op 1.50 [0.75–3.50] vs. 30 days 1.00 [0.00–3.00], p = 0.082). Volumetric perfusion analysis demonstrated reductions in lesion volumes for CBF (66.40 [43.35-145.70] → 28.55 [19.85-111.28] mL), MTT (220.75 [101.60-337.05] → 143.00 [39.93-242.35] mL), and Tmax (265.45 [145.53-333.63] → 212.40 [101.08-260.20] mL) on CT perfusion immediately postoperatively and at short-term follow-up, although these changes did not reach statistical significance (p = 0.068 for all). CBV lesion volume also decreased slightly (1.15 [0.25–5.51] → 0.00 [0.00–2.54] mL, p = 0.109).
Conclusion: Our results suggest that STA-MCA bypass surgery may offer clinical and hemodynamic benefits for ICAD patients who are unresponsive to medical and endovascular treatments. In this study, improved NIHSS and mRS scores, as well as hemodynamic parameters, were observed using CTP. Performing volumetric measurements may support the assessment of imaging outcomes. Given the small sample size and short follow-up period, these findings should be interpreted with caution. Large-scale and long-term studies are warranted to validate our findings and optimize ICAD treatment strategies.
Downloads
Metrics
References
Arenillas JF. Intracranial atherosclerosis: current concepts. Stroke 2011; 42: S20-3. DOI: https://doi.org/10.1161/STROKEAHA.110.597278
Gorelick PB, Wong KS, Bae HJ, Pandey DK. Large artery intracranial occlusive disease: a large worldwide burden but a relatively neglected frontier. Stroke 2008; 39: 2396–99. DOI: https://doi.org/10.1161/STROKEAHA.107.505776
Kim JS, Kang DW, Kwon SU. Intracranial atherosclerosis: incidence, diagnosis and treatment. J Clin Neurol 2005; 1: 1–7. DOI: https://doi.org/10.3988/jcn.2005.1.1.1
Wong LK. Global burden of intracranial atherosclerosis. Int J Stroke 2006; 1: 158–9. DOI: https://doi.org/10.1111/j.1747-4949.2006.00045.x
Meseguer E, Lavallée PC, Mazighi M, Labreuche J, Cabrejo L, Olivot JM et al. Yield of systematic transcranial Doppler in patients with transient ischemic attack. Ann Neurol 2010; 68: 9–17. DOI: https://doi.org/10.1002/ana.21921
Toyoda K, Yoshimura S, Nakai M, Koga M, Sasahara Y, Sonoda K et al. Twenty-year change in severity and outcome of ischemic and hemorrhagic strokes. JAMA Neurol 2022; 79: 61–9. DOI: https://doi.org/10.1001/jamaneurol.2021.4346
Cai S, Fan H, Peng C, Wu Y, Yang X. The comparison of STA-MCA bypass and BMT for symptomatic internal carotid artery occlusion disease: a systematic review and meta-analysis of long-term outcome. Chin Neurosurg J 2021; 7: 17. DOI: https://doi.org/10.1186/s41016-021-00236-2
Kataoka H, Miyamoto S, Ogasawara K, Iihara K, Takahashi JC, Nakagawara J et al. Results of prospective cohort study on symptomatic cerebrovascular occlusive disease showing mild hemodynamic compromise [Japanese Extracranial-Intracranial Bypass Trial (JET)- 2 Study]. Neurol Med Chir (Tokyo) 2015; 55: 460–8. DOI: https://doi.org/10.2176/nmc.oa.2014-0424
Powers WJ, Clarke WR, Grubb RL, Videen TO, Adams HP, Derdeyn CP. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: The carotid occlusion surgery study randomized trial. JAMA 2011; 306: 1983-92. DOI: https://doi.org/10.1001/jama.2011.1610
Guo L, Yang L, Li C, Zeng Y, Xu R, Wang Z, et al. The clinical outcome of emergency superficial temporal artery-to-middle cerebral artery bypass in acute ischemic stroke with large vessel occlusion. Neurosurg Rev 2024; 47: 25. DOI: https://doi.org/10.1007/s10143-023-02257-0
Sabouri M, Aminmansour B, Sourani A, Sharafi M, Sahraei A, Rahimi A, et al. The Role of early superficial temporal to middle cerebral artery bypass revascularization surgery in middle cerebral artery‐territory strokes: A systematic review study. Stroke Vasc Interv Neurol 2022; 2. DOI: https://doi.org/10.1161/SVIN.121.000281
Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. results of an international randomized trial. N Engl J Med 1985; 313: 1191–1200. DOI: https://doi.org/10.1056/NEJM198511073131904
The international cooperative study of extracranial/intracranial arterial anastomosis (EC/IC bypass study): methodology and entry characteristics. The EC/IC Bypass Study Group. Stroke 1985; 16: 397-406. DOI: https://doi.org/10.1161/01.STR.16.3.397
Ma Y, Wang T, Wang H, Amin-Hanjani S, Tong X, Wang J, et al. Extracranial-intracranial bypass and risk of stroke and death in patients with symptomatic artery Occlusion: The CMOSS Randomized Clinical Trial. JAMA 2023; 330: 704–14. DOI: https://doi.org/10.1001/jama.2023.22002
Li X, Li Y, Wang T, Sun X, Lu G, Xu X, et al. Determining the optimal age for extracranial-intracranial bypass surgery: A post hoc analysis of the CMOSS randomized trial. Stroke 2025; 56: 362–70. DOI: https://doi.org/10.1161/STROKEAHA.124.048766
Kuroda S, Kawabori M, Hirata K, Shiga T, Kashiwazaki D, Houkin K, et al. Clinical significance of STA-MCA double anastomosis for hemodynamic compromise in post-JET/ COSS era. Acta Neurochir (Wien), 2014; 156: 77-83. DOI: https://doi.org/10.1007/s00701-013-1961-0
Zhao H, Tong X, Wang X, Ding M, Zhang K. Ischemic stroke following STA-MCA double bypass. Transl Neurosci 2022; 13: 20–9. DOI: https://doi.org/10.1515/tnsci-2022-0211
Kan P, Srinivasan VM, Srivatsan A, Kaufmann AB, Cherian J, Burkhardt JK, et al. Double-barrel STA-MCA bypass for cerebral revascularization: lessons learned from a 10-year experience. J Neurosurg 2021; 135: 1385–93. DOI: https://doi.org/10.3171/2020.9.JNS201976
Kanamaru K, Araki T, Kawakita F, Hamada K, Kanamaru H, Matsuura K, et al. STAMCA bypass for the treatment of ischemic stroke. Acta Neurochir Suppl 2011; 112: 55–7. DOI: https://doi.org/10.1007/978-3-7091-0661-7_10
Chang X, Ruan X, Ding J, Ma P, Yang G, Zhang R, et al. The efficacy of STA-MCA double anastomosis comparing to single anastomosis in chronic internal carotid artery occlusion patients. Clin Neurol Neurosurg 2023; 233: 107947. DOI: https://doi.org/10.1016/j.clineuro.2023.107947
Low SW, Teo K, Lwin S, Yeo LL, Paliwal PR, Ahmad A, et al. Improvement in cerebral hemodynamic parameters and outcomes after superficial temporal artery-middle cerebral artery bypass in patients with severe stenoocclusive disease of the intracranial internal carotid or middle cerebral arteries. J Neurosurg 2015; 123: 662–9. DOI: https://doi.org/10.3171/2014.11.JNS141553
Jeffree RL, Stoodley MA. STA-MCA bypass for symptomatic carotid occlusion and haemodynamic impairment. J Clin Neurosci 2009; 16: 226–35. DOI: https://doi.org/10.1016/j.jocn.2008.01.022
Ning X jie, Gao Q, Chen C, Ling C, Liang J ji, Li Z yu, et al. Effects of superficial temporal artery-middle cerebral artery bypass on hemodynamics and clinical outcomes in the patients with atherosclerotic stenosis in the intracranial segment of internal carotid artery and middle cerebral artery. Clin Neurol Neurosurg 2019; 186: 105510. DOI: https://doi.org/10.1016/j.clineuro.2019.105510
Noh YH, Chung JW, Ko JH, Koo HW, Lee JY, Yoon SM, et al. Efficacy and safety of emergency extracranial-intracranial bypass for revascularization within 24 hours in resolving large artery occlusion with intracranial stenosis. World Neurosurg 2021; 155: e9–e18. DOI: https://doi.org/10.1016/j.wneu.2021.07.010
Teo KAC, Chou N, Lwin S, Yeo TT, Sharma VK. Long-term outcome in extracranialintracranial bypass surgery for severe stenoocclusive disease of intracranial internal carotid or middle cerebral artery. Clin Neurol Neurosurg 2018; 169: 149–53. DOI: https://doi.org/10.1016/j.clineuro.2018.04.003
Yoon S, Burkhardt JK, Lawton MT. Longterm patency in cerebral revascularization surgery: an analysis of a consecutive series of 430 bypasses. J Neurosurg 2018; 131: 80–7. DOI: https://doi.org/10.3171/2018.3.JNS172158
Konstas AA, Goldmakher G V., Lee TY, Lev MH. Theoretical basis and technical implementations of CT perfusion in acute ischemic stroke, part 1: Theoretic Basis. Am J Neuroradiol 2009; 30: 662–8. DOI: https://doi.org/10.3174/ajnr.A1487
Konstas AA, Goldmakher G V, Lee TY, Lev MH. Theoretical basis and technical implementations of CT perfusion in acute ischemic stroke, part 2: Technical Implementations. Am J Neuroradiol 2009; 30: 885–92. DOI: https://doi.org/10.3174/ajnr.A1492
Eicker SO, Beseoglu K, Etminan N, Turowski B, Steiger H-J, Hänggi D. The impact of early perfusion CT measurement after extracranial-intracranial bypass surgery: Results of a pilot study. Acta Neurochir Suppl: 2011: 112: 25-9. DOI: https://doi.org/10.1007/978-3-7091-0661-7_5
Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet 2000; 355: 1670–4. DOI: https://doi.org/10.1016/S0140-6736(00)02237-6
Pexman JH, Barber PA, Hill MD, Sevick RJ, Demchuk AM, Hudon ME, et al. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol 2001; 22: 1534–42.
Jo H, Lee SU, Jeong HG, Kim YD, Kim T, Sunwoo L, et al. Long-term outcomes and quantitative radiologic analysis of extracranial-intracranial bypass for hemodynamically compromised chronic large artery occlusive disease. Sci Rep 2023; 13: 3717. DOI: https://doi.org/10.1038/s41598-023-30874-8
Powers WJ, Martin WRW, Herscovitch P, Raichle ME, Grubb RL. Extracranial-intracranial bypass surgery: Hemodynamic and metabolic effects. Neurology 1984; 34: 1168–74. DOI: https://doi.org/10.1212/WNL.34.9.1168
Downloads
Additional Files
- Supplementary Criteria (Inclusion & Exclusion)
- Supplement 1 – NIHSS and mRS Scores
- Supplement 2 – 3D Brain Lesion Volume Metric (mL)
- Supplement 3 – Brain Lesion Volume (Pre vs Immediate Post-op)
- Supplement 4 – Brain Lesion Area (Pre vs Immediate Post-op)
- Supplement 5 – Brain Lesion Area (Pre vs Post-op 30 Days)
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







