CLINICAL MANAGEMENT OF SNAKEBITES IN COMMUNITY CARE UNIT: A SINGLE-CENTER RETROSPECTIVE STUDY IN LOPBURI, CENTRAL THAILAND
DOI:
https://doi.org/10.55374/jseamed.v9.204Keywords:
snakebite envenomation, epidemiology, clinical profile, snakebite management, antivenom availability, rural healthcare, ThailandAbstract
Background: Snakebite, a neglected tropical disease, might result in severe clinical outcomes.
Objectives: This study presents a retrospective analysis of snakebite data from a community hospital in Lopburi, Central Thailand, and also assesses snakebite distribution and clinical management to lower mortality and morbidity in the community setting.
Methods: A cross-sectional retrospective study used data from October 1, 2014, to August 30, 2023, to determine the epidemiology, clinical profile, and management of snakebite patients who visited Pattananikom Hospital.
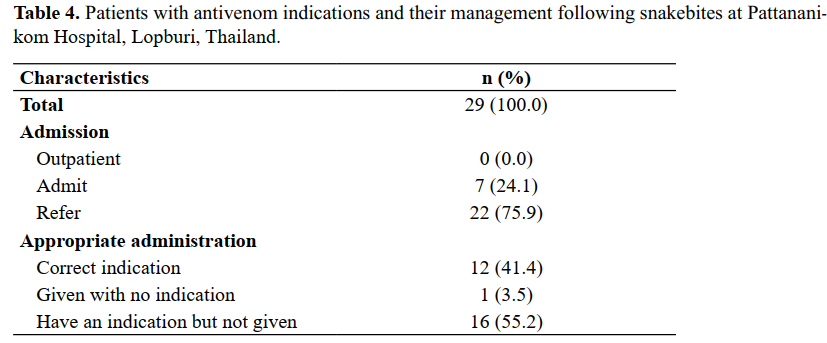
Results: The study included 225 snakebite patients with a median age of 39 (IQR 26-53 years), and 64.4% were male. The responsible species for half of the bite cases were unidentified (54.2%). Among 103 confirmed snakebites with identified species, there were 24 cobras (23.3%), 23 Russell’s vipers (22.3%), 16 green pit vipers (15.5%), 4 Malayan pit vipers (3.9%), 2 Malayan kraits (1.9%), and 34 (33.0%) other nonvenomous snakes. Notably, 10 out of 24 patients (41.7%) encountering cobras were diagnosed with venom ophthalmia. For bites caused by unknown snakes, two patients experienced compartment syndrome, one had dyspnea, and one had ptosis. Thirteen patients, also bitten by unidentified snakes and eligible for antivenom, went untreated due to a shortage of polyvalent antivenom, resulting in referrals. From 2021 to 2023, 20 patients (55.6% of 36) were referred (p=0.026). Of the patients with thrombocytopenia, eight (57.1% of 14) were referred (p=0.001), as were all cases with systemic bleeding, dyspnea, ptosis, or compartment syndrome. Moreover, prophylactic antibiotics (amoxicillin-clavulanate) were routinely prescribed (82.7%).
Conclusion: Snakebites have been referred to more frequently in the last three years. Even though the origins of most cases are unknown and often lead to referrals, there is a notable shortage of polyvalent antivenoms. This scarcity has the potential to delay treatment and increase the risk of mortality. This study highlights the need for improved antivenom access in community hospitals to mitigate delays and reduce mortality.
Downloads
Metrics
References
Vaiyapuri S, Kadam P, Chandrasekharuni G, Oliveira IS, Senthilkumaran S, Salim A, et al. Multifaceted community health education programs as powerful tools to mitigate snakebite-induced deaths, disabilities, and socioeconomic burden. Toxicon X 2023; 17: 100147. DOI: https://doi.org/10.1016/j.toxcx.2022.100147
Gutiérrez JM, Calvete JJ, Habib AG, Harrison RA, Williams DJ, Warrell DA. Snakebite envenoming. Nat Rev Dis Primers 2017; 3: 17063. DOI: https://doi.org/10.1038/nrdp.2017.63
Regional Action Plan for prevention and control of snakebite envenoming in the South-East Asia 2022–2030. New Delhi: World Health Organization, Regional Office for South-East Asia; 2022. Licence: CC BYNC-SA 3.0 IGO.
Patikorn C, Blessmann J, Nwe MT, Tiglao PJG, Vasaruchapong T, Maharani T et al. Estimating economic and disease burden of snakebite in ASEAN countries using a decision analytic model. PLoS Negl Trop Dis 2022; 16: e0010775. DOI: https://doi.org/10.1371/journal.pntd.0010775
Lertsakulbunlue S, Suebtuam R, Eamchotchawalit T, Chantkran W, Chaisakul J. Clinical profile and pharmacological management of snakebites in community care units: A retrospective study using two military hospital databases in South Thailand. Trop Med Infect Dis 2023; 8. DOI: https://doi.org/10.3390/tropicalmed8070346
WHO. Venomous snakes of the South-East Asia Region, their venoms and pathophysiology of human envenoming. Guidelines for the management of snakebites, 2nd edition. 2016;2.
Viravan C, Looareesuwan S, Kosakarn W, Wuthiekanun V, McCarthy CJ, Stimson AF, et al. A national hospital-based survey of snakes responsible for bites in Thailand. Trans R Soc Trop Med Hyg 1992; 86: 100–6. DOI: https://doi.org/10.1016/0035-9203(92)90463-M
Looareesuwan S, Vejcho S, Chanthavanich P, Supanaranond W, Phillips RE, Warrell DA et al. Clinical Significance of Venom Antigen Levels in Patients Envenomed by the Malayan Pit Viper (Calloselasma Rhodostoma). Am J Trop Med Hyg 1986; 35: 579–87. DOI: https://doi.org/10.4269/ajtmh.1986.35.579
Warrell DA. Snake bite. The Lancet 2010; 375: 77–88. DOI: https://doi.org/10.1016/S0140-6736(09)61754-2
Ratanabanangkoon K. Polyvalent Snake Antivenoms: Production Strategy and Their Therapeutic Benefits. Toxins (Basel) 2023; 15: 517. DOI: https://doi.org/10.3390/toxins15090517
de Silva HA, Ryan NM, de Silva HJ. Adverse reactions to snake antivenom, and their prevention and treatment. Br J Clin Pharmacol 2016; 81: 446–52. DOI: https://doi.org/10.1111/bcp.12739
Chesor M, Chaisakul J, Promsorn P, Chantkran W. Clinical laboratory investigations and antivenom administration after Malayan Pit Viper (Calloselasma rhodostoma) envenoming: A retrospective study from Southernmost Thailand. Am J Trop Med Hyg 2024; 110: 609–17. DOI: https://doi.org/10.4269/ajtmh.23-0657
Memon R, Erickson TB, Goldfine CE. Challenges in care of snake envenomation in rural Pakistan: a narrative review. Toxicol Commun 2023; 7. DOI: https://doi.org/10.1080/24734306.2023.2223049
Chaudhari T, Patil T, Paithankar M, Gulhane R, Patil M. Predictors of mortality in patients of poisonous snake bite: Experience from a tertiary care hospital in Central India. Int J Crit Illn Inj Sci 2014; 4: 101. DOI: https://doi.org/10.4103/2229-5151.134145
Lertsakulbunlue S, Kunsuwan P, Rangsin R, Sakboonyarat B. Pulmonary tuberculosis mortality and its risk factors among patients with type 2 diabetes and pulmonary tuberculosis in four community hospitals, central Thailand. J Southeast Asian Med Res 2022; 6: e0120. DOI: https://doi.org/10.55374/jseamed.v6i0.120
Rojnuckarin P, Suteparak S, Sibunruang S. Review article. Diagnosis and management of venomous snakebites in Southeast Asia. Asian Biomed 2017; 6: 795–805.
Tangtrongchitr T, Thumtecho S, Janprasert J, Sanprasert K, Tongpoo A, Tanpudsa Y, et al. Malayan pit viper envenomation and treatment in Thailand. Ther Clin Risk Manag 2021; 17: 1257–66. DOI: https://doi.org/10.2147/TCRM.S337199
Timerga A, Kelta E, Kenenisa C, Zawdie B, Habte A, Haile K. Serum electrolytes disorder and its associated factors among adults admitted with metabolic syndrome in Jimma Medical Center, South West Ethiopia: Facility based cross-sectional study. PLoS One 2020; 15: e0241486. DOI: https://doi.org/10.1371/journal.pone.0241486
Lilliefors HW. On the Kolmogorov-Smirnov Test for normality with mean and variance unknown. J Am Stat Assoc 1967; 62: 399. DOI: https://doi.org/10.2307/2283970
Wongtongkam N, Wilde H, Sitthi-Amorn C, Ratanabanangkoon K. A study of Thai Cobra ( Naja kaouthia ) bites in Thailand. Mil Med 2005; 170: 336–341. DOI: https://doi.org/10.7205/MILMED.170.4.336
Wongtongkam N, Wilde H, Sitthi-Amorn C, Ratanabanangkoon K. A Study of 225 Malayan pit viper bites in Thailand. Mil Med 2005; 170: 342–48. DOI: https://doi.org/10.7205/MILMED.170.4.342
Othong R, Eurcherdkul T, Chantawatsharakorn P. Green pit viper envenomations in Bangkok: A comparison of follow-up compliance and clinical outcomes in older and younger adults. Toxins (Basel) 2022; 14: 869. DOI: https://doi.org/10.3390/toxins14120869
Young BA, Boetig M, Westhoff G. Functional bases of the spatial dispersal of venom during cobra “spitting”. Physiol Biochem Zool 2009; 82: 80–9. DOI: https://doi.org/10.1086/595589
Rasmussen S, Young B, Krimm H. On the ‘spitting’ behaviour in cobras (Serpentes: Elapidae). J Zool 1995; 237: 27–35. DOI: https://doi.org/10.1111/j.1469-7998.1995.tb02743.x
Berthé RA, de Pury S, Bleckmann H, Westhoff G. Spitting cobras adjust their venom distribution to target distance. J Comp Physiol 2009; 195: 753–7. DOI: https://doi.org/10.1007/s00359-009-0451-6
Tansuwannarat P, Tongpoo A, Phongsawad S, Sriapha C, Wananukul W, Trakulsrichai S. A retrospective cohort study of cobra envenomation: clinical characteristics, treatments, and outcomes. Toxins (Basel) 2023; 15: 468. DOI: https://doi.org/10.3390/toxins15070468
Ratnapalan S, Das L. Causes of eye burns in children. Pediatr Emerg Care 2011; 27: 151–6. DOI: https://doi.org/10.1097/PEC.0b013e318209f08c
Jalink M. Ocular complications of spitting cobra venom. Indian J Ophthalmol 2020; 68: 2632. DOI: https://doi.org/10.4103/ijo.IJO_1164_20
Chang K-C, Huang Y-K, Chen Y-W, Chen M-H, Tu AT, Chen Y-C. Venom ophthalmia and ocular complications caused by snake venom. Toxins (Basel) 2020; 12: 576. DOI: https://doi.org/10.3390/toxins12090576
Ang L, Sangtam T, Sanjay S. Ophthalmia due to spitting cobra venom in an urban setting - A report of three cases. Middle East Afr J Ophthalmol 2014; 21: 259. DOI: https://doi.org/10.4103/0974-9233.134689
Senthilkumaran S, Almeida JR, Williams J, Salim A, Williams HF, Thirumalaikolundusubramanian P, et al. Russell’s viper envenomation induces rectus sheath haematoma. Toxicon 2023; 224: 107037. DOI: https://doi.org/10.1016/j.toxicon.2023.107037
Slagboom J, Kool J, Harrison RA, Casewell NR. Haemotoxic snake venoms: their functional activity, impact on snakebite victims and pharmaceutical promise. Br J Haematol 2017; 177: 947–59. DOI: https://doi.org/10.1111/bjh.14591
Pillai LV, Ambike D, Husainy S, Khaire A, Captain A, Kuch U. Severe neurotoxic envenoming and cardiac complications after the bite of a ‘Sind Krait’ (Bungarus cf. sindanus) in Maharashtra, India. Trop Med Health 2012; 40: 103–108. DOI: https://doi.org/10.2149/tmh.2012-08c
Kularatne SAM. Common krait (Bungarus caeruleus ) bite in Anuradhapura, Sri Lanka: a prospective clinical study, 1996–98. Postgrad Med J 2002; 78: 276–80. DOI: https://doi.org/10.1136/pmj.78.919.276
Aye K-P, Thanachartwet V, Soe C, Desakorn V, Thwin K-T, Chamnanchanunt S, et al. Clinical and laboratory parameters associated with acute kidney injury in patients with snakebite envenomation: a prospective observational study from Myanmar. BMC Nephrol 2017; 18: 92. DOI: https://doi.org/10.1186/s12882-017-0510-0
Bhattacharya S, Krishnamurthy A, Gopalakrishnan M, Kalra S, Kantroo V, Aggarwal S, et al. Endocrine and Metabolic Manifestations of Snakebite Envenoming. Am J Trop Med Hyg 2020; 103: 1388–96. DOI: https://doi.org/10.4269/ajtmh.20-0161
Lertsakulbunlue S, Khimmaktong W, Khow O, Chantkran W, Noiphrom J, Promruangreang K, et al. Snake venom pharmacokinetics and acute toxic outcomes following Daboia siamensis envenoming: experimental and clinical correlations. Toxins (Basel) 2024; 17: 10. DOI: https://doi.org/10.3390/toxins17010010
Thumtecho S, Tangtrongchitr T, Srisuma S, Kaewrueang T, Rittilert P, Pradoo A, et al. Hematotoxic manifestations and management of green pit viper bites in Thailand. Ther Clin Risk Manag 2020; 16: 695–704. DOI: https://doi.org/10.2147/TCRM.S261303
Patikorn C, Ismail AK, Abidin SAZ, Blanco FB, Blessmann J, Choumlivong K, et al. Situation of snakebite, antivenom market and access to antivenoms in ASEAN countries. BMJ Glob Health 2022; 7: e007639. DOI: https://doi.org/10.1136/bmjgh-2021-007639
Isbister GK. Antivenom availability, delays and use in Australia. Toxicon X 2023; 17: 100145. DOI: https://doi.org/10.1016/j.toxcx.2022.100145
Houcke S, Pujo JM, Vauquelin S, Lontsi Ngoula GR, Matheus S, NkontCho F, et al. Effect of the time to antivenom administration on recovery from snakebite envenoming-related coagulopathy in French Guiana. PLoS Negl Trop Dis 2023; 17: e0011242. DOI: https://doi.org/10.1371/journal.pntd.0011242
WHO. World Health Organization (WHO) Regional Office in South-East Asia. Guidelines for Management of Snakebites, 2nd ed.; WHO Regional Office in South-East Asia: New Delhi, India, 2016. 2016.
Isbister GK. Antivenom availability, delays and use in Australia. Toxicon X 2023; 17: 100145. DOI: https://doi.org/10.1016/j.toxcx.2022.100145
Isbister GK, Chiew AL, Buckley NA, Soderstrom J, Brown SGA, Jenkins S, et al. Real world delays in antivenom administration: patient, snake or hospital factors (ASP-33). Clin Toxicol 2024; 1–6. DOI: https://doi.org/10.1080/15563650.2024.2433125
Silva A, Hlusicka J, Siribaddana N, Waiddyanatha S, Pilapitiya S, Weerawansa P, et al. Time delays in treatment of snakebite patients in rural Sri Lanka and the need for rapid diagnostic tests. PLoS Negl Trop Dis 2020; 14: e0008914. DOI: https://doi.org/10.1371/journal.pntd.0008914
Sachett JAG, da Silva IM, Alves EC, Oliveira SS, Sampaio VS, do Vale FF, et al. Poor efficacy of preemptive amoxicillin clavulanate for preventing secondary infection from Bothrops snakebites in the Brazilian Amazon: A randomized controlled clinical trial. PLoS Negl Trop Dis 2017; 11: e0005745. DOI: https://doi.org/10.1371/journal.pntd.0005745
Résière D, Olive C, Kallel H, Cabié A, Névière R, Mégarbane B, et al. Oral microbiota of the snake Bothrops lanceolatus in Martinique. Int J Environ Res Public Health 2018; 15: 2122. DOI: https://doi.org/10.3390/ijerph15102122
Palappallil DS. Pattern of use of antibiotics following snake bite in a tertiary care hospital. J Clin Diagnos Res 2015; 9: OCO5-9. DOI: https://doi.org/10.7860/JCDR/2015/14753.6322
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







