RISING TRENDS IN CURRENT TOBACCO USE AMONG ACTIVE-DUTY PERSONNEL OF THE ROYAL THAI ARMY IN THAILAND FROM 2017 TO 2022 AND ITS ASSOCIATED METABOLIC RISK FACTORS FOR CARDIOVASCULAR DISEASE IN 2022
DOI:
https://doi.org/10.55374/jseamed.v8.198Keywords:
Tobacco use, prevalence, blood pressure, hyperglycemia, hypertriglyceridemiaAbstract
Background: Tobacco use is a well-established risk factor for developing cardiovascular disease (CVD). In recent years, the prevalence of metabolic risk factors for CVD has been increasing among Royal Thai Army (RTA) personnel in Thailand. Despite a decline in tobacco use, an essential lifestyle risk factor, among Thai civilians from 2015 to 2020, it is unclear how common it is among RTA personnel.
Objectives: This study aimed to determine the trends of current tobacco use among active-duty RTA personnel from 2017 to 2022 and to evaluate the association between tobacco use and metabolic risk factors for CVD among this population in 2022.
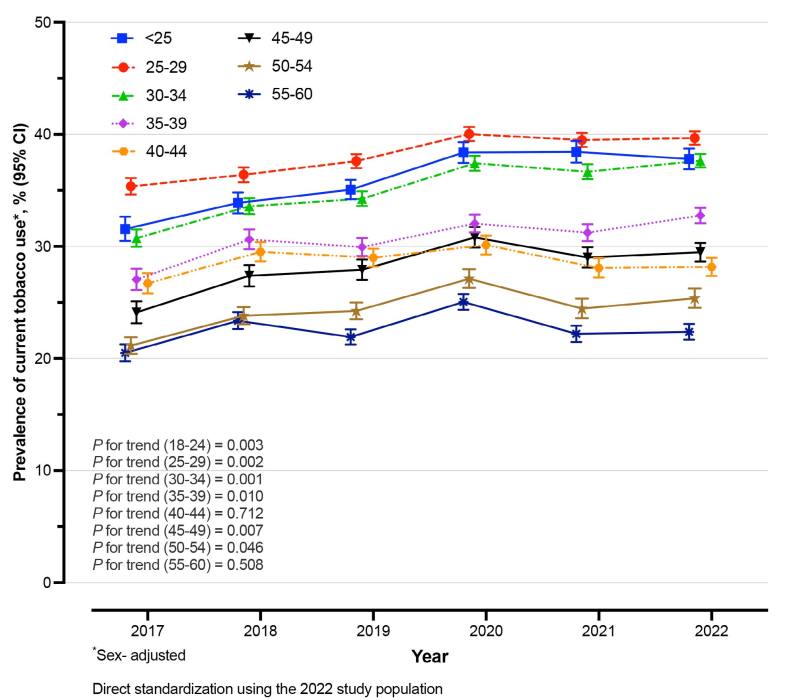
Methods: A serial cross-sectional study was carried out using data from the annual health examination database of RTA personnel from 2017 to 2022. The study included 614,198 active-duty RTA personnel aged 20-60. Current tobacco use was defined as smoking within the previous 12 months. Each year’s adjusted current tobacco use prevalence was estimated using direct standardization to the 2022 study population as a reference. The multivariable logit model was used to evaluate the association between tobacco use and metabolic risk factors for CVD in 2022, presented as an adjusted prevalence ratio (APR) and 95% confidence interval (CI).
Results: The age- and sex-adjusted prevalence of current tobacco use among RTA personnel increased from 28.4% (95% CI: 28.1-28.7) in 2017 to 33.2% (95% CI: 33.9-33.4) in 2022, p for trend = 0.021. In men, the age-adjusted prevalence of current tobacco use was 31.8% in 2017 and increased to 36.5% in 2022, p for trend = 0.032. For women, it was 1.1% in 2017 and rose to 5.7% in 2022, p for trend = 0.032. A significant association between current tobacco use and the prevalence of metabolic risk factors for CVD was observed, including diastolic blood pressure ≥ 90 mmHg (APR 1.04; 95% CI 1.01-1.07), fasting plasma glucose ≥ 126 mmHg (APR 1.26; 95% CI 1.18-1.34), and triglyceridemia ≥ 150 mg/dL (APR 1.28; 95% CI 1.25-1.31).
Conclusion: The prevalence of current tobacco use among active-duty RTA personnel increased from 2017 to 2022. Additionally, a significant association between tobacco use and metabolic risk factors for CVD was observed. Tobacco cessation should be facilitated in this population to attenuate the risk of CVD later.
Downloads
Metrics
References
World Health Organization. Noncommunicable diseases [Internet]. 2022 [cited 2023 May 3]. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
Khan SS, Ning H, Sinha A, Wilkins J, Allen NB, Vu THT, et al. Cigarette smoking and competing risks for fatal and nonfatal cardiovascular disease subtypes across the life course. J Am Heart Assoc 2021; 10: e021751. DOI: https://doi.org/10.1161/JAHA.121.021751
Jee SH, Foong AW, Hur NW, Samet JM. Smoking and risk for diabetes incidence and mortality in Korean men and women. Diabetes Care 2010; 33: 2567–72.
Jacob L, Freyn M, Kalder M, Dinas K, Kostev K. Impact of tobacco smoking on the risk of developing 25 different cancers in the U.K.: a retrospective study of 422,010 patients followed for up to 30 years. Oncotarget 2018; 9: 17420. DOI: https://doi.org/10.18632/oncotarget.24724
Kitjakrancharoensin P, Yasan K, Hongyantarachai K, Ratanachokthorani K, Thammasarn J, Kuwuttiwai D, et al. Prevalence and risk factors of chronic obstructive pulmonary disease among agriculturists in a rural community, central Thailand. Int J Chron Obstruct Pulmon Dis 2020; 15: 2189. DOI: https://doi.org/10.2147/COPD.S262050
WHO global report on trends in prevalence of tobacco smoking 2000-2025. World Health Organization; 2018.
Aekplakorn W. Thai National Health Examination Survey V (2014) [Internet]. 2014 [cited 2023 Oct 3]. Available from: https://www.hsri.or.th/researcher/research/new-release/detail/7711
Aekplakorn W. Thai National Health Examination Survey VI (2019-2020) [Internet]. 2019 [cited 2023 Oct 3]. Available from: https://online.fliphtml5.com/bcbgj/znee/#p=187
Sakboonyarat B, Rangsin R, Mittleman MA. Incidence and risk factors of metabolic syndrome among Royal Thai Army personnel. Sci Rep 2022; 12: 1-11. DOI: https://doi.org/10.1038/s41598-022-19024-8
Sakboonyarat B, Poovieng J, Jongcherdchootrakul K, Srisawat P, Hatthachote P, Mungthin M, et al. Rising trends in obesity prevalence among Royal Thai Army personnel from 2017 to 2021. Sci Rep 2022; 12: 7726.
Sakboonyarat B, Poovieng J, Srisawat P, Hatthachote P, Mungthin M, Rangsin R, et al. Prevalence, awareness, and control of hypertension and associated factors among Royal Thai Army personnel in Thailand from 2017 to 2021. Sci Rep 2023; 13: 6946. DOI: https://doi.org/10.1038/s41598-023-34023-z
Sakboonyarat B, Sangkool T, Poovieng J, Jongcherdchootrakul K, Srisawat P, Hatthachote P, et al. Trend in the prevalence of type 2 diabetes among Royal Thai Army personnel and associated factors from 2017 to 2021. J Southeast Asian Med Res 2023; 7: e0160. DOI: https://doi.org/10.55374/jseamed.v7.160
Sakboonyarat B, Poovieng J, Jongcherdchootrakul K, Srisawat P, Hatthachote P, Mungthin M, et al. Trends in Serum total cholesterol and high total cholesterol prevalence among royal Thai army personnel in Thailand, 2017–2022. High Blood Press Cardiovasc Prev 2023; 1-12. DOI: https://doi.org/10.1038/s41598-022-11913-2
Sakboonyarat B, Poovieng J, Jongcherdchootrakul K, Srisawat P, Hatthachote P, Mungthin M, et al. Prevalence of hypertriglyceridemia among Royal Thai Army personnel and its related cardiometabolic risk factors, from 2017 to 2021. BMC Public Health 2022; 22: 1569. DOI: https://doi.org/10.1186/s12889-022-13992-2
Sakboonyarat B, Poovieng J, Jongcherdchootrakul K, Srisawat P, Hatthachote P, Mungthin M, et al. Rising trends in the predicted 10-year risk of cardiovascular diseases among Royal Thai Army personnel from 2017 to 2021. Sci Rep 2023; 13: 1476. DOI: https://doi.org/10.1038/s41598-023-28494-3
Ngamjarus C. n4Studies: sample size calculation for an epidemiological study on a smart device. Siriraj Med J 2016; 68: 160-70.
Kunanon S, Chattranukulchai P, Chotruangnapa C, Kositanurit W, Methavigul K, Boonyasirinant T, et al. 2019 Thai Guidelines on the Treatment of Hypertension: ExecutiveS. J Med Assoc Thai 2021; 104: 1729-38. DOI: https://doi.org/10.35755/jmedassocthai.2021.10.12199
Widome R, Joseph AM, Polusny MA, Chlebeck B, Brock B, Gulden A, et al. Talking to Iraq and Afghanistan war veterans about tobacco use. Nicotine Tob Res 2011; 13: 623-26. DOI: https://doi.org/10.1093/ntr/ntr028
Talcott GW, Cigrang J, Sherrill-Mittleman D, Snyder DK, Monty Baker M, Tatum JL, et al. Tobacco use during military deployment. Nicotine Tob Res 2013; 15: 1348-54. DOI: https://doi.org/10.1093/ntr/nts267
Al-Khashan HI, al Sabaan FS, al Nasser HS, al Buraidi AA, al Awad AD, Horaib GB, et al. The prevalence of smoking and its associated factors among military personnel in Kingdom of Saudi Arabia: A national study. J Family Community Med 2014; 21: 147-53. DOI: https://doi.org/10.4103/2230-8229.142966
Smith EA, Malone RE. Mediatory myths in the U.S. military: tobacco use as “stress relief.” Am J Health Promot 2014; 29: 115-22. DOI: https://doi.org/10.4278/ajhp.121009-QUAL-491
Lee WB, Fong GT, Zanna MP, Borland R, Omar M, Sirirassamee B. Regret and rationalization among smokers in Thailand and Malaysia: findings from the International Tobacco Control Southeast Asia Survey. Health Psychol 2009; 28: 457. DOI: https://doi.org/10.1037/a0014669
Hosking W, Borland R, Yong HH, Fong G, Zanna M, Laux F, et al. The effects of smoking norms and attitudes on quitting intentions in Malaysia, Thailand and four Western nations: a cross-cultural comparison. Psychol Health 2009; 24: 95-107. DOI: https://doi.org/10.1080/08870440802385854
Omvik P. How smoking affects blood pressure. Blood Pressure 1996; 5: 71-7. DOI: https://doi.org/10.3109/08037059609062111
Virdis A, Giannarelli C, Fritsch Neves M, Taddei S, Ghiadoni L. Cigarette smoking and hypertension. Curr Pharm Des 2010; 16: 2518-25. DOI: https://doi.org/10.2174/138161210792062920
Seifu Y, Tsegaw D, Haji Y, Ejeso A. Prevalence and associated factors of diabetes mellitus among adult population in Hawassa Zuria Woreda, Sidama Region, Ethiopia. Diabetes Metab Syndr Obes 2020; 13: 4571-79. DOI: https://doi.org/10.2147/DMSO.S275230
Maddatu J, Anderson-Baucum E, EvansMolina C. Smoking and the risk of type 2 diabetes. Transl Res 2017; 184: 101-7. DOI: https://doi.org/10.1016/j.trsl.2017.02.004
Clair C, Bitton A, Meigs JB, Rigotti NA. Relationships of cotinine and self-reported cigarette smoking with hemoglobin A1c in the U.S.: results from the National Health and Nutrition Examination Survey, 1999-2008. Diabetes Care 2011; 34: 2250-55. DOI: https://doi.org/10.2337/dc11-0710
Jee SH, Foong AW, Hur NW, Samet JM. Smoking and risk for diabetes incidence and mortality in Korean men and women. Diabetes Care 2010; 33: 2567-72. DOI: https://doi.org/10.2337/dc10-0261
Kelly TN, Bazzano LA, Fonseca VA, Thethi TK, Reynolds K, He J. Systematic review: glucose control and cardiovascular disease in type 2 diabetes. Ann Intern Med 2009; 151: 394-403. DOI: https://doi.org/10.7326/0003-4819-151-6-200909150-00137
Control TD, Group CTDR. Effect of intensive diabetes management on macrovascular events and risk factors in the Diabetes Control and Complications Trial. Am J Cardiol 1995; 75: 894-903. DOI: https://doi.org/10.1016/S0002-9149(99)80683-3
Kim SK, Kim HC, Shim JS, Kim DJ. Effects of cigarette smoking on blood lipids in Korean men: Cardiovascular and metabolic diseases etiology research center cohort. Korean J Intern Med 2020; 35: 369. DOI: https://doi.org/10.3904/kjim.2019.133
Al-Aubaidy HA, Jelinek HF. Oxidative stress and triglycerides as predictors of subclinical atherosclerosis in prediabetes. Redox Report 2014; 19: 87-91. DOI: https://doi.org/10.1179/1351000213Y.0000000080
Tanriverdi H, Evrengul H, Kuru O, Tanriverdi S, Seleci D, Enli Y, et al. Cigarette smoking induced oxidative stress may impair endothelial function and coronary blood flow in angiographically normal coronary arteries. Circ J 2006; 70: 593-9. DOI: https://doi.org/10.1253/circj.70.593
Moradinazar M, Pasdar Y, Najafi F, Shahsavari S, Shakiba E, Hamzeh B, et al. Association between dyslipidemia and blood lipids concentration with smoking habits in the Kurdish population of Iran. BMC Public Health 2020; 20: 1-10. DOI: https://doi.org/10.1186/s12889-020-08809-z
Lando HA. Promoting Tobacco Cessation in Low- and Middle-Income Countries. J Smok Cessat 2016; 11: 66-9. DOI: https://doi.org/10.1017/jsc.2016.7
Soulakova JN, Tang CY, Leonardo SA, Taliaferro LA. Motivational benefits of social support and behavioral interventions for smoking cessation. J Smok Cessat 2018; 13: 216-26. DOI: https://doi.org/10.1017/jsc.2017.26
Aubin H, Luquiens A, Berlin I. Pharmacotherapy for smoking cessation: pharmacological principles and clinical practice. Br J Clin Pharmacol 2014; 77: 324-36. DOI: https://doi.org/10.1111/bcp.12116
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







