INTERVENTION TO IMPROVE MEDICAL ADHERENCE IN PEDIATRIC KIDNEY TRANSPLANT RECIPIENTS
DOI:
https://doi.org/10.55374/jseamed.v8.218Keywords:
Medical non-adherence, Pediatric kidney transplantation, BAASIS questionnaire, Intervention, %CVAbstract
Background: Adolescent age at transplantation has long been recognized as a risk factor for graft failure, and a major contributor might be medical nonadherence. Many interventions have been applied to improve adherence in adults. However, there is limited data about intervention in pediatric kidney transplant recipients.
Objectives: The study aimed to study the improvement of medical adherence in pediatric kidney transplant recipients after receiving the intervention and to evaluate the associated factors to medical nonadherence
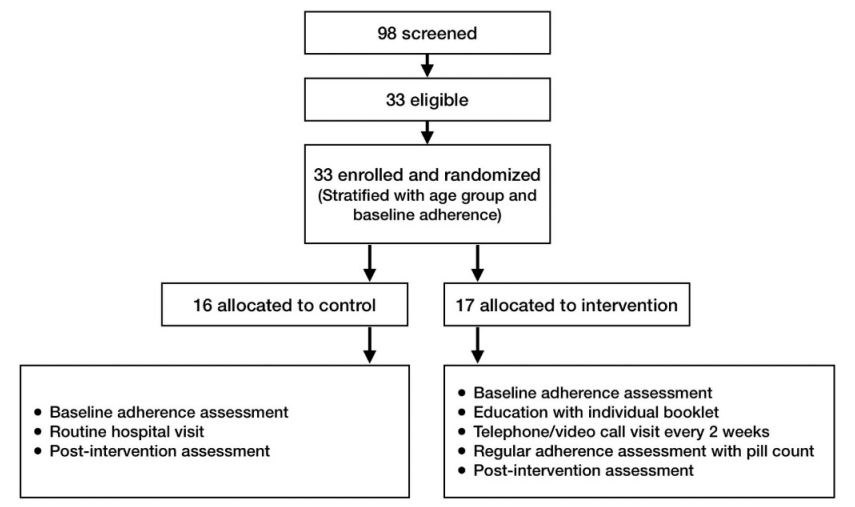
Methods: A single-center randomized controlled trial was conducted on pediatric kidney transplant recipients at Phramongkutklao Hospital, aged below 21 years, with at least one year post-transplantation and without acute rejection within three months. Randomization was 1:1. The intervention included educational sessions with individual booklets, telephone calls, or video call visits every two weeks, with regular assessment of adherence. Adherence was assessed using the Basel Assessment of Adherence to Immunosuppressive Medications Scale (BAASIS) and the coefficient of variation (CV%) of tacrolimus level.
Results: Thirty-three patients were eligible: 17 for intervention and 16 for control. The mean age was 15.7±3.12 years. Nonadherence prevalence at baseline was 30.3% by questionnaire and 40.7% by %CV. After one year, the total number of non-adherents decreased to 21.2% using the questionnaire and 15.4% using %CV, but there was no difference between the intervention and control groups. After performing a multivariate analysis to evaluate the factors associated with medical nonadherence, no factor was significantly associated. However, some factors, such as the total number of prescribed drugs, tended to be significant (p = 0.071 and 0.331 using univariate and multivariate analysis, respectively).
Conclusion: The prevalence of medical nonadherence in pediatric kidney transplant recipients is higher than in adults. Medical nonadherence is complex; interventions must be individualized and done with a multidisciplinary team. Keywords: medical nonadherence
Downloads
Metrics
References
Thai Transplant Society. Registry book 2021. Print & More company limited 2565; 1: 43-63.
Rianthavorn P, Kerr SJ, Lumpaopong A, Jiravuttipong A, Pattaragarn A, Tangnararatchakit K, et al. Outcomes and predictive factors of pediatric kidney transplants: an analysis of the Thai Transplant Registry. Pediatr Transplant. 2013; 17: 112–8. DOI: https://doi.org/10.1111/petr.12047
Foster BJ, Dahhou M, Zhang X, Platt RW, Samuel SM, Hanley JA, et al. Association between age and graft failure rates in young kidney transplant recipients. Transplantation 2011; 92: 1237-43. DOI: https://doi.org/10.1097/TP.0b013e31823411d7
Dobbels F, Ruppar T. Adherence to the immunosuppressive regimen in pediatric kidney transplant recipients: A systematic review. Pediatr Transplantation 2010; 14: 603-13. DOI: https://doi.org/10.1111/j.1399-3046.2010.01299.x
Rao PS. Survival on dialysis post-kidney transplant failure: results from the scientific registry of transplant recipients. Am J Kidney Dis 2007; 49: 294-300. DOI: https://doi.org/10.1053/j.ajkd.2006.11.022
Foster BJ, Pai LH, Zelikovsky N, Amaral S, Bell L, Dharnidharka VR, et al. A randomized trial of a multicomponent intervention to promote medication adherence: the teen adherence in kidney transplant effectiveness of intervention trial (TAKE-IT). Am J Kidney Dis 2018; 72: 30-41. DOI: https://doi.org/10.1053/j.ajkd.2017.12.012
Schmid A, Hils S, Kramer-Zucker A, Bogatyreva L, Hauschke D, De Geest S, et al. Telemedically supported case management if living-donor renal transplant recipients to optimize routine evidence-based aftercare; a single-center randomized controlled trial. Am J Transplant 2017; 17: 1594-605. DOI: https://doi.org/10.1111/ajt.14138
Andrew N, Barraclough KA, Long K, Fazio TN, Holt S, Kanhutu K, et al. Telehealth model of care for routine follow up of renal transplant recipients in a tertiary centre: a case study. J Telemed Telecare 2020; 26: 232-8. DOI: https://doi.org/10.1177/1357633X18807834
University of Basel. The Basel assessment of adherence to immunosuppressive medications scale (BAASIS). Switzerland: University of Basel; 2021.
Neu MA. Special issues in pediatric kidney transplantation. Adv Chronic Kidney Dis 2006; 13: 62-9. DOI: https://doi.org/10.1053/j.ackd.2005.10.001
Pizzo HP, Ettenger RB, Gjertson DW, Reed EF, Zhang J, Gritsch HA, et al. Sirolimus and tacrolimus coefficient of variation is associated with rejection, donor-specific antibodies, and nonadherence. Pediatr Nephrol 2016; 31: 2345–52. DOI: https://doi.org/10.1007/s00467-016-3422-5
Rapoff MA. Adherence to Pediatric Medical Regimens. 2th ed. New York. Springer Science+Business; 2010. DOI: https://doi.org/10.1007/978-1-4419-0570-3
Wangpradit P, Larpparisuth N. Prevalence and predictive factors of nonadherence among Thai kidney transplant patients. The 35th annual meeting of the Royal College of Physicians of Thailand.
Sabate AL. Adherence to long-term therapies: Evidence for action. Geneva: World Health Organization; 2003.
Neuberger JM, Bechstein WO, Kuypers DRJ, Burra P, Citterio F, De Geest S, et al. Practical recommendations for long-term management of modifiable risks in kidney and liver transplant recipients: a guidance report and clinical checklist by the consensus on managing modifiable risk in transplantation (COMMIT) group. Transplantation 2017; 101: S1-56. DOI: https://doi.org/10.1097/TP.0000000000001651
Steinberg EA, Moss M, Buchanan CL. Adherence in pediatric kidney transplant recipients. Pediatr Nephrol 2018; 33: 361-72. DOI: https://doi.org/10.1007/s00467-017-3637-0
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







