ACCURACY OF SUSCEPTIBILITY WEIGHTED IMAGING AND 3D-TOF MRA IN DETECTION AND PRE-TREATMENT EVALUATION OF INTRACRANIAL DURAL ARTERIOVENOUS FISTULAS
DOI:
https://doi.org/10.55374/jseamed.v8.192Keywords:
dural arteriovenous fistulas (DAVFs), three-dimensional time-of-flight magnetic resonance angiography (3D-TOF MRA), susceptibility-weighted imaging (SWI), fistulous point, cortical venous reflux (CVR), cortical venous ectasia (CVE)Abstract
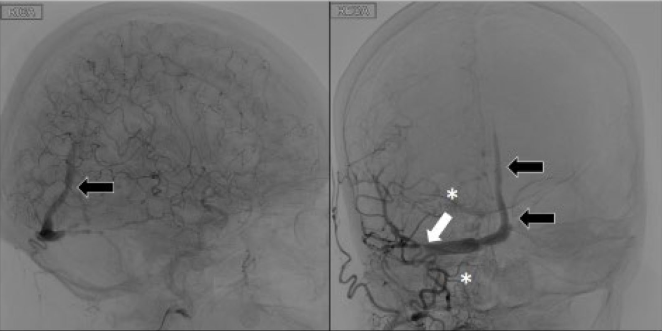
Background: Dural arteriovenous fistulas (DAVFs) are abnormal connections between meningeal arteries and dural venous sinuses or cortical veins. A cerebral angiogram is the gold standard for diagnosing and treating DAVFs. Still, non-invasive techniques such as three-dimensional time-offlight magnetic resonance angiography (3D-TOF MRA) and susceptibility-weighted imaging (SWI) are also helpful in evaluating the location and severity of the fistulas, including cortical venous reflux (CVR) and cortical venous ectasia (CVE). This study aimed to compare the efficacy in detecting and pretreating DAVFs evaluating SWI and 3D-TOF MRA with cerebral angiography.
Methods: The retrospective study included 35 patients with 41 DAVFs who underwent pre-treatment MR imaging and cerebral angiogram. The fistulous point at convexity and cavernous locations, arterial feeders, venous drainers, CVR, and CVE were evaluated.
Results: SWI and 3D-TOF MRA showed high sensitivity and excellent specificity in detecting DAVFs Cognard II-IV at convexity location and high sensitivity in evaluating CVR. For DAVFs at cavernous sinus locations, arterial feeders and venous drainers were significantly identified in 3D-TOF MRA (p < 0.001). SWI exhibited superior sensitivity (87.5%) in detecting CVE at convexity locations (p < 0.001). Slow flow or low-grade fistulas in cavernous sinus locations (n = 2, 4.8%, Cognard I) were not identified using MR imaging.
Conclusion: SWI and 3D-TOF MRA are helpful tools for evaluating high-flow DAVFs (Cognard II-IV). SWI is superior in detecting CVE in convexity locations but is limited in assessing the fistulous point in cavernous sinus locations. Thus, combining findings from both SWI and 3D-TOF MRA exhibited high accuracy in detecting and pretreating high-flow DAVFs.
Downloads
Metrics
References
Kim MS, Han DH, Kwon OK, Oh CW, Han MH. Clinical characteristics of dural arteriovenous fistula. J Clin Neurosci 2002; 9: 147-55. https://doi.org/10.1054/jocn.2001.1029 DOI: https://doi.org/10.1054/jocn.2001.1029
Lasjaunias P, Chiu M, ter Brugge K, Tolia A, Hurth M, Bernstein M. Neurological manifestations of intracranial dural arteriovenous malformations. J Neurosurg 1986; 64: 724-30. https://doi.org/10.3171/jns.1986.64.5.0724 DOI: https://doi.org/10.3171/jns.1986.64.5.0724
Lin YH, Lin HH, Liu HM, Lee CW, Chen YF. Diagnostic performance of CT and MRI on the detection of symptomatic intracranial dural arteriovenous fistula: a meta-analysis with indirect comparison. Neuroradiology 2016; 58: 753-63. https://doi.org/10.1007/s00234-016-1696-8 DOI: https://doi.org/10.1007/s00234-016-1696-8
Newton TH, Cronqvist S. Involvement of dural arteries in intracranial arteriovenous malformations. Radiology 1969; 93: 1071-8. https://doi.org/10.1148/93.5.1071 DOI: https://doi.org/10.1148/93.5.1071
Söderman M, Pavic L, Edner G, Holmin S, Andersson T. Natural history of dural arteriovenous shunts. Stroke 2008; 39: 1735-9. https://doi.org/10.1161/STROKEAHA.107.506485 DOI: https://doi.org/10.1161/STROKEAHA.107.506485
Gross BA, Du R. The natural history of cerebral dural arteriovenous fistulae. Neurosurgery 2012; 71: 594-602. discussion -3. https://doi.org/10.1227/NEU.0b013e31825eabdb DOI: https://doi.org/10.1227/NEU.0b013e31825eabdb
van Dijk JM, terBrugge KG, Willinsky RA, Wallace MC. Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke 2002; 33: 1233- 6. https://doi.org/10.1161/01.STR.0000014772.02908.44 DOI: https://doi.org/10.1161/01.STR.0000014772.02908.44
Kaufmann TJ, Huston J, 3rd, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF. Complications of diagnostic cerebral angiography: evaluation of 19,826 consecutive patients. Radiology 2007; 243: 812-9. https://doi.org/10.1148/radiol.2433060536 DOI: https://doi.org/10.1148/radiol.2433060536
Cloft HJ, Joseph GJ, Dion JE. Risk of cerebral angiography in patients with subarachnoid hemorrhage, cerebral aneurysm, and arteriovenous malformation: a meta-analysis. Stroke 1999; 30: 317-20. https://doi.org/10.1161/01.STR.30.2.317 DOI: https://doi.org/10.1161/01.STR.30.2.317
Meckel S, Maier M, Ruiz DS, Yilmaz H, Scheffler K, Radue EW, et al. MR angiography of dural arteriovenous fistulas: diagnosis and follow-up after treatment using a time-resolved 3D contrast-enhanced technique. AJNR Am J Neuroradiol 2007; 28: 877-84.
Azuma M, Hirai T, Shigematsu Y, Kitajima M, Kai Y, Yano S, et al. Evaluation of intracranial dural arteriovenous fistulas: comparison of unenhanced 3T 3D time-of-flight MR angiography with digital subtraction angiography. Magn Reson Med Sci 2015; 14: 285- 93. https://doi.org/10.2463/mrms.2014-0120 DOI: https://doi.org/10.2463/mrms.2014-0120
Churojana A, Lakkhanawat S, Chailerd O, Boonchai T, Cognard CC. Cranial dural arteriovenous fistulas: can noninvasive imaging predict angiographic findings? Siriraj Medical J 2018; 70: 289-97.
Haacke EM, Xu Y, Cheng YC, Reichenbach JR. Susceptibility weighted imaging (SWI). Magn Reson Med 2004; 52: 612-8. https://doi.org/10.1002/mrm.20198 DOI: https://doi.org/10.1002/mrm.20198
Haacke EM, Mittal S, Wu Z, Neelavalli J, Cheng YC. Susceptibility-weighted imaging: technical aspects and clinical applications, part 1. AJNR Am J Neuroradiol 2009; 30: 19- 30. https://doi.org/10.3174/ajnr.A1400 DOI: https://doi.org/10.3174/ajnr.A1400
Hodel J, Gerber S, Zins M, Rodallec M, Leclerc X, Blanc R, et al. MR imaging findings in intracranial dural arteriovenous fistula shunt with retrograde cortical venous drainage using susceptibility-weighted angiography. AJNR Am J Neuroradiol 2011; 32: E196-7. https://doi.org/10.3174/ajnr.A2875 DOI: https://doi.org/10.3174/ajnr.A2875
Letourneau-Guillon L, Krings T. Simultaneous arteriovenous shunting and venous congestion identification in dural arteriovenous fistulas using susceptibility-weighted imaging: initial experience. AJNR Am J Neuroradiol 2012; 33: 301-7. https://doi.org/10.3174/ajnr.A2777 DOI: https://doi.org/10.3174/ajnr.A2777
Jagadeesan BD, Delgado Almandoz JE, Moran CJ, Benzinger TL. Accuracy of susceptibility-weighted imaging for the detection of arteriovenous shunting in vascular malformations of the brain. Stroke 2011; 42: 87-92. https://doi.org/10.1161/STROKEAHA.110.584862 DOI: https://doi.org/10.1161/STROKEAHA.110.584862
Saini J, Thomas B, Bodhey NK, Periakaruppan A, Babulal JM. Susceptibility-weighted imaging in cranial dural arteriovenous fistulas. Am J Neuroradiol 2009; 30: e6-e. https://doi.org/10.3174/ajnr.A1265 DOI: https://doi.org/10.3174/ajnr.A1265
Nakagawa I, Taoka T, Wada T, Nakagawa H, Sakamoto M, Kichikawa K, et al. The use of susceptibility-weighted imaging as an indicator of retrograde leptomeningeal venous drainage and venous congestion with dural arteriovenous fistula: diagnosis and follow-up after treatment. Neurosurg 2013; 72: 47-54; discussion 5. https://doi.org/10.1227/NEU.0b013e318276f7cc DOI: https://doi.org/10.1227/NEU.0b013e318276f7cc
Jain NK, Kannath SK, Kapilamoorthy TR, Thomas B. The application of susceptibility -weighted MRI in pre-interventional evaluation of intracranial dural arteriovenous fistulas. J Neurointerv Surg 2017; 9: 502-7. https://doi.org/10.1136/neurintsurg-2016-012314 DOI: https://doi.org/10.1136/neurintsurg-2016-012314
Chen JC, Tsuruda JS, Halbach VV. Suspected dural arteriovenous fistula: results with screening MR angiography in seven patients. Radiology 1992; 183: 265-71. https://doi.org/10.1148/radiology.183.1.1549684 DOI: https://doi.org/10.1148/radiology.183.1.1549684
Farb RI, Agid R, Willinsky RA, Johnstone DM, Terbrugge KG. Cranial dural arteriovenous fistula: diagnosis and classification with time-resolved MR angiography at 3T. Am J Neuroradiol 2009; 30: 1546-51 https://doi.org/10.3174/ajnr.A1646 DOI: https://doi.org/10.3174/ajnr.A1646
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.