PASSIVE LEG RAISING EFFECT AT RESUSCITATION AMONG PATIENTS WITH VASOPLEGIC STATE
DOI:
https://doi.org/10.55374/jseamed.v5i2.100Keywords:
Vasoplegia, Cardiac output, Venous return, Mean systemic pressureAbstract
Background: Several dynamic parameters have been used clinically to predict volume responsiveness and to guide fluid administration of which passive leg raising (PLR) is one of the most reliable techniques. PLR induces rising in cardiac output attributes through an unstressed volume mobilization from legs to heart causing autologous preload increment. Appropriate fluid resuscitation is essential and can be optimized by hemodynamic-based approach to vasodilatory hypotension.
Objective: This study aimed to evaluate the effectiveness and safety of PLR at early resuscitation among patients with vasoplegia.
Methods: We conducted a comparison study concerning an experimental design using a single blinded assessment of the outcomes that assigned patients with shock to be treated with PLR or flat position at early resuscitation. Forty patients with shock were included in this study. Twenty patients performed PLR at early resuscitation compared with the others that performed in the flat position and were measured for cardiac output (CO), mean arterial pressure (MAP), diastolic blood pressure (DBP), heart rate (HR), central venous pressure (CVP) and systemic vascular resistance (SVR) immediately after the procedures. The primary outcome was to evaluate the effect of early PLR on hemodynamic variables among hypotensive patients by comparing the difference in CO while the secondary outcomes were differences in MAP, DBP, HR, CVP, SVR, survival at hospital admission and the pulmonary complications of chest x-rays between the two groups.
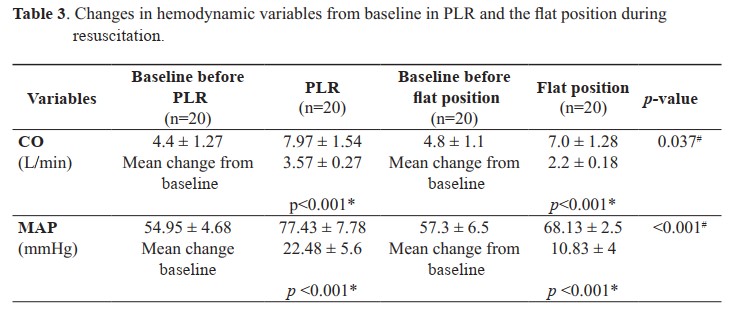
Results: No difference was observed in baseline characteristics between the two groups of patients. Compared with the flat position, PLR at early resuscitation significantly increased CO (3.57 ± 0.27 vs. 2.2 ± 0.18 L/min, p = 0.037), MAP (22.48 ± 5.6 vs. 10.83 ± 4 mmHg, p<0.001), DBP (19 ± 0.20 vs. 1.23 ± 0.12 mmHg, p=0.001) and CVP (4.52 ± 0.19 vs. 2.18 ± 0.13 mmHg, p=0.002). However, no differences were observed in HR, SVR, pulmonary complications of chest X-rays [2 (10%) vs. 1 (5%), p = 0.23] as well as survival at hospital admission [16 (80%) vs. 13 (65%), p = 0.48] between the two groups.
Conclusion: Among patients with shock, PLR at early resuscitation significantly increased CO, MAP, DBP and CVP than that of those performing the flat position. No differences were found in HR, SVR, pulmonary complications; PLR did not improve survival to hospital admission.
Downloads
Metrics
References
Standards and guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiac Care (ECC). JAMA 1986; 255: 2905–84. DOI: https://doi.org/10.1001/jama.1986.03370210073024
Rutlen DL, Wackers FJ, Zaret BL. Radionuclide assessment of peripheral intravascular capacity: a technique to measure intravascular volume changes in the capacitance circulation in man. Circulation 1981; 64: 146–52. DOI: https://doi.org/10.1161/01.CIR.64.1.146
Yang Z, Tang D, Wu X, Hu X, Xu J, Qian J, et al. A tourniquet assisted cardiopulmonary resuscitation augments myocardial perfusion in a porcine model of cardiac arrest. Resuscitation 2015; 86: 49–53. DOI: https://doi.org/10.1016/j.resuscitation.2014.10.009
Monnet X, Teboul J-L. Passive leg raising. Intensive Care Med 2008; 34: 659–63. DOI: https://doi.org/10.1007/s00134-008-0994-y
Dragoumanos V, Iacovidou N, Chalkias A, Lelovas P,Koutsovasilis A, Papalois A, et al. Passive leg raising during cardiopulmonary resuscitation results in improved neurological outcome in a swine model of prolonged ventricular fibrillation. Am J Emerg Med 2012; 30: 1935–42. DOI: https://doi.org/10.1016/j.ajem.2012.04.014
Keller G, Desebbe O, Benard M, Bouchet JB, Lehot JJ. Bedside assessment of PLR effects on venous return. J Clin Monit Comput 2011; 25: 257–63.
Bernard SA, Smith K, Finn J, Hein C, Grantham H, Bray JE, et al. Induction of therapeutic hypothermia during out-of-hospital cardiac arrest using a rapid infusion of cold saline: the RINSE trial (Rapid Infusion of Cold Normal Saline). Circulation 2016; 134: 797–805. DOI: https://doi.org/10.1161/CIRCULATIONAHA.116.021989
Kim F, Nichol G, Maynard C, Hallstrom A, Kudenchuk PJ, Rea T, et al. Effect of prehospital induction of mild hypothermia on survival and neurological status among adults with cardiac arrest: a randomized clinical trial. JAMA 2014; 311: 45. DOI: https://doi.org/10.1001/jama.2013.282173
Holmén J, Herlitz J, Jimenez-Herrera M, Karlsson T, Axelsson C. Passive leg raising in out-of-hospital cardiac arrest. Resuscitation 2019; 137: 94–101. DOI: https://doi.org/10.1016/j.resuscitation.2019.02.017
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, et al. Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 2006; 34: 1402–7. DOI: https://doi.org/10.1097/01.CCM.0000215453.11735.06
Chalkias A, Xanthos T. Pathophysiology and pathogenesis of post resuscitation myocardial stunning. Heart Fail Rev 2011; 17: 117–28. DOI: https://doi.org/10.1007/s10741-011-9255-1
Ditchey RV. Potential adverse effects of volume loading on perfusion of vital organs during closed-chest resuscitation.Circulation 1984; 69: 181–9. DOI: https://doi.org/10.1161/01.CIR.69.1.181
Paradis NA. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA 1990; 263: 1106. DOI: https://doi.org/10.1001/jama.1990.03440080084029
Axelsson C, Holmberg S, Karlsson T, Axelssonå B, Herlitz J. Passive leg raising during cardiopulmonary resuscitation in out-of-hospital cardiac arrest—Does it improve circulation and outcome? Resuscitation 2010; 81: 1615–20. DOI: https://doi.org/10.1016/j.resuscitation.2010.08.019
Guérin L, Teboul JL, Persichini R, Dres M, Richard C, Monnet X. Effects of passive leg raising and volume expansion on mean systemic pressure and venous return in shock in humans. Crit Care 2015; 19: 411. DOI: https://doi.org/10.1186/s13054-015-1115-2
Mitchell M. levy, Laura E. Evans, Andrew Rhodes. The surviving sepsis campaign bundle:2018 update. Intensive Care Med 2018; 44: 925-28. DOI: https://doi.org/10.1007/s00134-018-5085-0
Laurent Guerin, Jean-Louis, Romain Persichini, Effect of passive leg raising and volume expansion on mean systemic pressure and venous return. J Anesthesiol 2018; 71: 386-93.
Monnet X, Teboul JL. Passive leg raising: five rules, not a drop of fluid. Crit Care 2015; 19: 18. DOI: https://doi.org/10.1186/s13054-014-0708-5
Keller G, Desebbe O, Benard M, Bouchet JB, Lehot JJ. Bedside assessment of passive leg raising effects on venous return. J Clin Monit Comput 2011; 25: 257–63. DOI: https://doi.org/10.1007/s10877-011-9303-3
Malbrain ML, Reuter DA. Assessing fluid responsiveness with the passive leg raising maneuver in patients with increased intraabdominal pressure: be aware that not all blood returns Crit Care Med 2010; 38: 1912–5. DOI: https://doi.org/10.1097/CCM.0b013e3181f1b6a2
Mahjoub Y, Touzeau J, Airapetian N, Lorne E, Hijazi M, Zogheib E, et al. The passive leg-raising maneuver cannot accurately predict fluid responsiveness in patients with intra-abdominal hypertension. Crit Care Med 2010; 38: 1824–9. DOI: https://doi.org/10.1097/CCM.0b013e3181eb3c21
Teboul JL. Mean systemic pressure: we can now estimate it, but for what. Intensive Care Med 2013; 39: 1487–8. DOI: https://doi.org/10.1007/s00134-013-2979-8
Yoshioka A, Nishimura K, Seki K, Onodera N Effects of passive leg raising on cross sectional area of inferior vena cava and stroke volume. Kawasaki Med Welfare J 2010; 19: 285-90.
Wong DH, O’Connor D, Tremper KK, Zaccari J, Thompson P, et al. Changes in cardiac output after acute blood loss and position change in man. Crit Care Med 1989; 17: 979-83. DOI: https://doi.org/10.1097/00003246-198910000-00002
RoddieIC, Shepherd JT. The effects of carotid artery compression in man with special reference to changes in vascular resistance in the limbs. J Physiol 1957; 139: 377-84. DOI: https://doi.org/10.1113/jphysiol.1957.sp005898
Barbieri R, Triedman JK, Saul JP. Heart rate control and mechanical cardiopulmonary coupling to assess central volume: a systems analysis. Am J Physiol Regul Integr Comp Physiol 2002; 283: R1210-20. DOI: https://doi.org/10.1152/ajpregu.00127.2002
Parati G, Grassi G, Coruzzi P, Musiari L, Ravogli A, et al. Influence of cardiopulmonary receptors on the bradycardic responses to carotid baroreceptor stimulation in man. Clin Sci (Lond) 1987; 72: 639-45. DOI: https://doi.org/10.1042/cs0720639
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.