AIRFLOW, BEHAVIORS AND DELAYED DETECTION: DRIVERS OF A COVID-19 OUTBREAK IN A THAI MILITARY RECRUIT TRAINING UNIT, MAY-JUNE 2025
DOI:
https://doi.org/10.55374/jseamed.v9.262Keywords:
COVID-19, outbreak investigation, military recruit training unit, airflow, delayed detectionAbstract
Background: On May 6, 2025, the Epidemiology Unit of Phramongkutklao Hospital was notified of a probable COVID-19 outbreak among recruits and instructors at a recruit training unit in Samut Sakhon Province, Thailand. A joint field investigation was conducted in collaboration with the 11th Medical Unit, the Epidemiology Unit of Phramongkutklao Hospital, and the Armed Forces Research Institute of Medical Sciences (AFRIMS).
Objective: To confirm and characterize the COVID-19 outbreak, identify critical gaps in the existing protocol and transmission factors, and provide recommendations for control and prevention.
Methods: A retrospective cohort study was conducted from May 1 to June 3, 2025. Cases included individuals with at least two COVID-19–compatible symptoms, a positive antigen test kit (ATK) result, or laboratory confirmation by real-time RT-PCR. Structured interviews and standardized questionnaires collected exposure and behavior data. A walk-through survey assessed environmental conditions, including airflow, temperature, and humidity in the dormitory. Outbreak control measures, including cohorting based on ATK results, were documented.
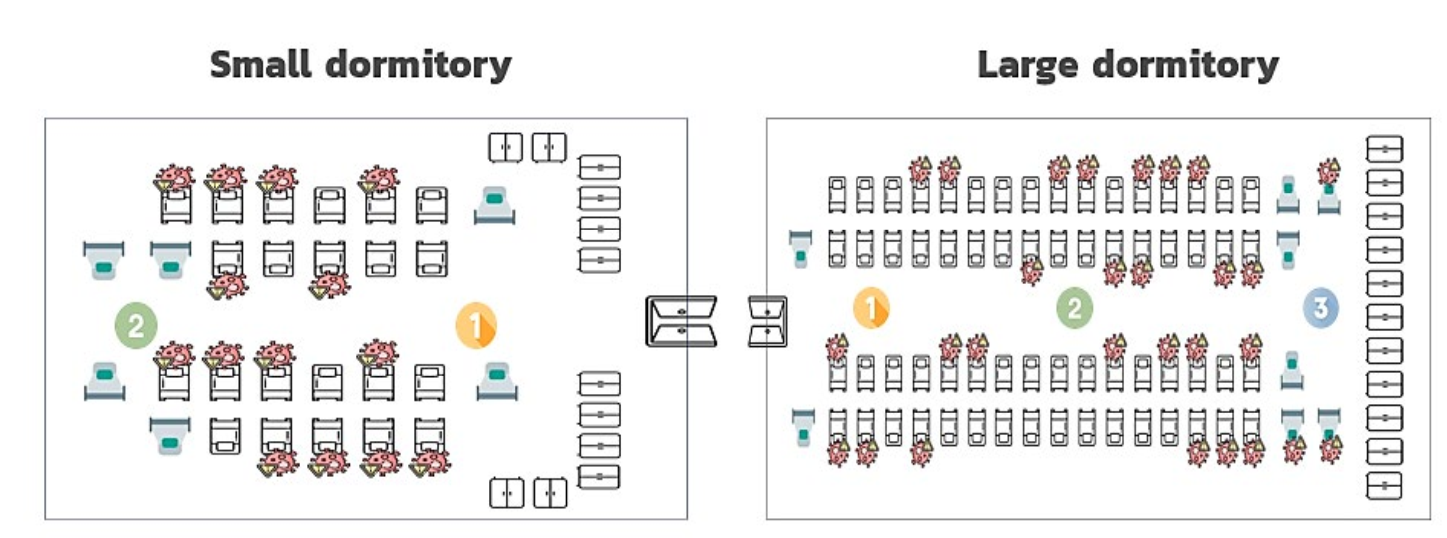
Results: Among 114 personnel, 47 cases were identified (attack rate 41.2%), with 97.9% symptomatic. Of these, 95.7% had received prior COVID-19 vaccination. Common symptoms were sore throat, headache, and cough. The environmental assessment showed elevated temperatures, humidity, and west-to-east airflow, which correlated with higher attack rates in the eastern sleeping zones. Behavioral factors included shared drinking glasses and proximity during meals; sharing glasses showed the lowest p-value (adjusted OR = 1.99, 95% CI: 0.89–4.48). Delayed detection due to a lack of systematic screening facilitated transmission.
Conclusions: The outbreak was driven by multifactorial causes, including delayed detection and environmental and behavioral factors. Alignment between airflow and attack rates highlights the role of ventilation. Proactive surveillance, systematic ATK screening for all respiratory symptoms, and enforcement of physical distancing are recommended to prevent similar outbreaks in congregate military settings.
Downloads
Metrics
References
World Health Organization. Coronavirus disease (COVID-19) pandemic [Internet]. Geneva: World Health Organization; 2020 [cited 2025 Aug 15]. Available from: https://www.who.int/emergencies/diseases/novelcoronavirus-2019/covid-19-pandemic
Department of Disease Control, Ministry of Public Health, Thailand. Guidelines for surveillance, prevention, and control of COVID-19. Bangkok: Department of Disease Control, Ministry of Public Health; 2022.
Kim JH, An JA, Min PK, Bitton A, Gawande AA. COVID-19 outbreak and response in the South Korean military. Am J Prev Med 2020; 59: e211–4.
Ladner JT, Larsen BB, Bowers JR, Zangari T, Miller C, Kadingo O, et al. Investigation of a SARS-CoV-2 outbreak in a U.S. Marine Corps recruit training facility. N Engl J Med 2021; 384: 2407–16. DOI: https://doi.org/10.1056/NEJMc2032165
World Health Organization (WHO). Transmission of SARS-CoV-2: implications for infection prevention precautions. Scientific Brief, Jul 9 2020. Geneva: World Health Organization; 2020.
Department of Disease Control, Ministry of Public Health, Thailand. COVID-19 situation report: outbreak in military and training units. Bangkok: Department of Disease Control, Ministry of Public Health; 2021.
Seow J, Lee SY, Tang JW, Looi D, Ling L, Puan KJ, et al. Outbreak of COVID-19 in the Singapore Armed Forces: epidemiological characteristics and control strategies. Mil Med 2021; 186: e256–63.
Department of Medical Services (Thailand). Guidance for diagnosis, treatment and prevention of COVID-19 in hospitals (Revised version 27) [Internet]. Bangkok: Department of Medical Services; 2023 Apr 18 [cited 2025 Nov 27]. Available from: https://covid19.dms.go.th/Content/Select_Landding_page?-contentId=181
Ngambunchai J, Jongkrathok P, Phisitpayat N, Prommongkol J, Saenmai S, Saisut C, et al. Investigation of a COVID-19 outbreak among new recruits at a military training unit, Mueang Buriram District, Buriram Province, April–May 2024. WESR [Internet]. 2025 Mar 31 [cited 2025; 56: e3350. Available from: https://he05.tci-thaijo.org/index.php/WESR/article/view/3350
Department of Health, Ministry of Public Health, Thailand. Announcement of indoor air quality surveillance standards in public buildings B.E. 2565. Bangkok: Department of Health, Ministry of Public Health; 2022.
Department of Disease Control, Ministry of Public Health, Thailand. Digital Disease Surveillance platform [Internet]. Bangkok: Department of Disease Control, Ministry of Public Health; [date unknown] [cited 2025 Aug 15]. Available from: https://ddsdoe.ddc.moph.go.th/ddss/
Thongsawang T, Sawangsrisutikul K, Hongchan P, Plernprom P, Thongsom P, Pingkan P, et al. Risk of coronavirus disease 2019 (COVID-19) in special military operations in southern Thailand, 2021; 16: 87–92. DOI: https://doi.org/10.59096/osir.v16i2.263708
Li F, Jiang G, Hu T. Coughing intensity and wind direction effects on the transmission of respiratory droplets: A computation with Euler–Lagrange method. Atmosphere 2022; 13: 594. DOI: https://doi.org/10.3390/atmos13040594
Mohammadi L, Mehravaran A, Derakhshan Z, Gharehchahi E, Bontempi E, Golaki M, et al. Investigating the role of environmental factors on the survival, stability, and transmission of SARS-CoV-2, and their contribution to COVID-19 outbreak: A review. Sustainability 2022; 14: 11135. DOI: https://doi.org/10.3390/su141811135
Wang J, Tang K, Feng K, Ye T, Lu Y, Ding F, et al. Impact of temperature and relative humidity on the transmission of COVID-19: a modelling study in China and the United States. BMJ Open 2021; 11: e043863. DOI: https://doi.org/10.1136/bmjopen-2020-043863
Gong Z, Song T, Hu M, Ma S, Li B, Zhang M, et al. Natural and socio-environmental factors in the transmission of COVID-19: a comprehensive analysis of epidemiology and mechanisms. BMC Public Health 2024; 24: 2196. DOI: https://doi.org/10.1186/s12889-024-19749-3
World Health Organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. Scientific brief [Internet]. Geneva: World Health Organization; 2020 Mar 29 [cited 2025 Aug 23]. Available from: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causingCOVID-19-implications-for-ipc-precautionrecommendations
Saulnier A, Wendling JM, Hermant B, Lepelletier D. SARS-CoV-2 transmission modes: why and how contamination occurs around shared meals and drinks? Food Microbiol 2023; 114: 104297. DOI: https://doi.org/10.1016/j.fm.2023.104297
Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARSCoV-2 as compared with SARS-CoV-1. N Engl J Med 2020; 382: 1564–7. DOI: https://doi.org/10.1056/NEJMc2004973
Chin AWH, Chu JTS, Perera MRA, Hui KPY, Yen H-L, Chan KH, et al. Stability of SARSCoV-2 in different environmental conditions. Lancet Microbe. 2020; 1: e10. DOI: https://doi.org/10.1016/S2666-5247(20)30003-3
Byambasuren O, Stehlik P, Clark J, Alcorn K, Glasziou P. Effect of COVID-19 vaccination on long COVID: systematic review. BMJ Med 2023; 2: e000621. DOI: https://doi.org/10.1136/bmjmed-2022-000385
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







