Clinical Features and Risk Factors for Severe Disease of Rickettsiosis: A Military Hospital-Based Study in Bangkok, Thailand
DOI:
https://doi.org/10.55374/jseamed.v8.212Keywords:
rickettsiosis, murine typhus, scrub typhusAbstract
Background: Rickettsiosis is Southeast Asia’s third leading cause of undifferentiated fever. Due to limited epidemiological data and nonspecific symptoms, diagnosing the disease is complex, leading to treatment challenges and complications. Military personnel are at a higher risk for rickettsial exposure, and their treatment might be delayed due to military duties.
Objectives: The study aimed to investigate the outbreak, symptoms, and clinical manifestations of rickettsiosis, as well as the risk factors for severe disease, among patients treated at the military hospital in Bangkok, Thailand.
Methods: A retrospective analysis of rickettsiosis’s epidemiology, symptoms, and clinical manifestations was performed. The data were collected from patient electronic medical records at Phramongkutklao Hospital from June 2009 to May 2020.
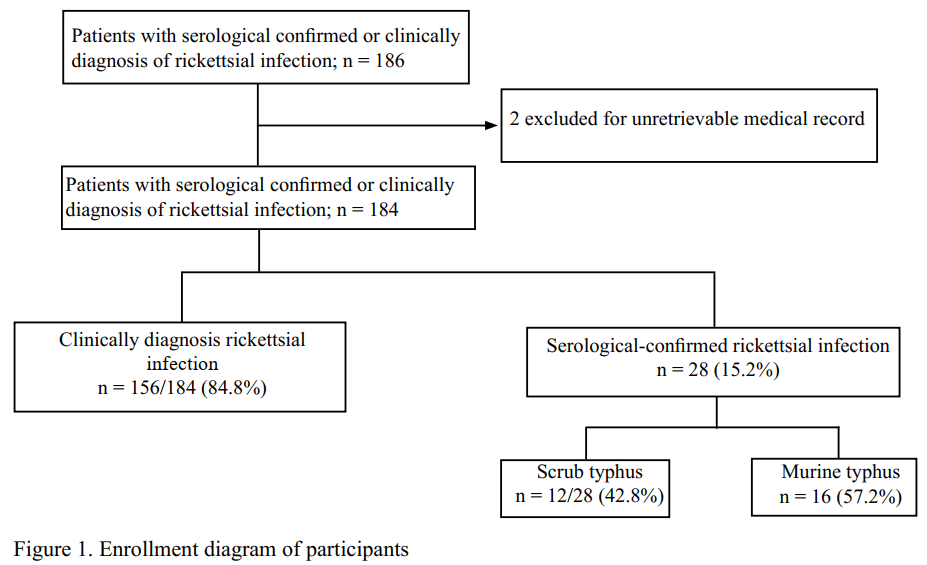
Results: Of 184 confirmed patients diagnosed with rickettsial infection, 12 scrub typhus, 16 murine typhus, and 156 were clinically diagnosed with rickettsiosis. Nineteen cases (10%) were grouped as severe rickettsial infection, and the other 165 (90%) were in the non-severe group. Fever, myalgia, rigor, and headache were common presentations of rickettsiosis. Alteration of consciousness and tachypnea were common in those with severe rickettsiosis group. Impaired renal function, elevated bilirubin, elevated alkaline phosphatases, aspartate aminotransferase, and alanine aminotransferase, pyuria, as well as abnormal chest radiographs, were more common findings in the severe rickettsiosis group. Additionally, the rate of ICU admission (73.7% vs. 8.5%, p < 0.001) and duration of hospitalization (18.63 ± 20 vs. 7.42 ± 7.58, p < 0.026) were significantly higher in the severe rickettsiosis group. The mortality rate of rickettsiosis was 2.1%. Elevated bilirubin (OR = 17.93, 95% CI = 3.52-91.42, p = 0.001) and abnormal chest radiograph (OR = 11.73, 95% CI = 1.36-100.89, p = 0.025) were independently predictive for severe disease.
Conclusion: Murine typhus was more common in a military hospital in Bangkok and less severe than scrub typhus. Increased bilirubin levels and abnormal chest radiography with bilateral alveolar infiltration tend to predict severe rickettsial infection independently.
Downloads
Metrics
References
Vincent G. Scrub typhus and its causative agent, Orientia tsutsugamushi: Rickettsiales. 2016 13 September: 329-72. DOI: https://doi.org/10.1007/978-3-319-46859-4_16
Xu G, Walker DH, Jupiter D, Melby PC, Arcari CM. A review of the global epidemiology of scrub typhus. PLoS Negl Trop Dis 2017; 11: e0006062. DOI: https://doi.org/10.1371/journal.pntd.0006062
Vanramliana, Pautu L, Lalmalsawma P, Rosangkima G, Sarma DK, Chinzah H, et al. Epidemiology of scrub typhus and other rickettsial infections (2018-22) in the hyperendemic setting of Mizoram, North-East India. PLoS Negl Trop Dis 2023; 17: e0011688. DOI: https://doi.org/10.1371/journal.pntd.0011688
Qian L, Wang Y, Wei X, Liu P, Magalhaes RJS, Qian Q, et al. Epidemiological characteristics and spatiotemporal patterns of scrub typhus in Fujian province during 2012-2020. PLoS Negl Trop Dis 2022; 16: e0010278. DOI: https://doi.org/10.1371/journal.pntd.0010278
Faruque LI, Zaman RU, Gurley ES, Massung RF, Alamgir AS, Galloway RL, et al. Prevalence and clinical presentation of Rickettsia, Coxiella, Leptospira, Bartonella and chikungunya virus infections among hospital-based febrile patients from December 2008 to November 2009 in Bangladesh. BMC Infect Dis 2017; 17: 141. DOI: https://doi.org/10.1186/s12879-017-2239-6
Stewart AGA, Smith S, Binotto E, McBride WJH, Hanson J. The epidemiology and clinical features of rickettsial diseases in North Queensland, Australia: Implications for patient identification and management. PLoS Negl Trop Dis 2019; 13: e0007583. DOI: https://doi.org/10.1371/journal.pntd.0007583
Luvira V, Silachamroon U, Piyaphanee W, Lawpoolsri S, Chierakul W, Leaungwutiwong P, et al. Etiologies of acute undifferentiated febrile illness in Bangkok, Thailand. Am J Trop Med Hyg 2019; 100: 622-9. DOI: https://doi.org/10.4269/ajtmh.18-0407
Satjanadumrong J, Robinson MT, Hughes T, Blacksell SD. Distribution and ecological drivers of spotted fever group rickettsia in Asia. EcoHealth 2019; 16: 611-26. DOI: https://doi.org/10.1007/s10393-019-01409-3
Caravedo Martinez MA, Ramírez-Hernández A, Blanton LS. Manifestations and management of flea-borne rickettsioses. Res Rep Trop Med 2021; 12: 1-14. DOI: https://doi.org/10.2147/RRTM.S274724
Parola P, Miller RS, McDaniel P, Telford SR, 3rd, Rolain JM, Wongsrichanalai C, et al. Emerging rickettsioses of the Thai-Myanmar border. Emerg Infect Dis 2003; 9: 592-5. DOI: https://doi.org/10.3201/eid0905.020511
Suputtamongkol Y, Suttinont C, Niwatayakul K, Hoontrakul S, Limpaiboon R, Chierakul W, et al. Epidemiology and clinical aspects of rickettsioses in Thailand. Ann N Y Acad Sci 2009; 1166: 172-9. DOI: https://doi.org/10.1111/j.1749-6632.2009.04514.x
Luce-Fedrow A, Lehman ML, Kelly DJ, Mullins K, Maina AN, Stewart RL, et al. A Review of scrub typhus (Orientia tsutsugamushi and related Organisms): then, now, and tomorrow. Trop Med Infect Dis 2018; 3: 8. DOI: https://doi.org/10.3390/tropicalmed3010008
Premaratna R, Loftis AD, Chandrasena TG, Dasch GA, de Silva HJ. Rickettsial infections and their clinical presentations in the Western Province of Sri Lanka: a hospital-based study. Int J Infect Dis 2008; 12: 198-202. DOI: https://doi.org/10.1016/j.ijid.2007.06.009
Trung NV, Hoi LT, Dien VM, Huong DT, Hoa TM, Lien VN, et al. Clinical manifestations and molecular diagnosis of scrub typhus and murine typhus, Vietnam, 2015-2017. Emerg Infect Dis 2019; 25: 633-41. DOI: https://doi.org/10.3201/eid2504.180691
Eldin C, Parola P. Rickettsioses as causes of CNS infection in southeast Asia. Lancet Glob Health 2015; 3: e67-8. DOI: https://doi.org/10.1016/S2214-109X(14)70379-1
Peter JV, Sudarsan TI, Prakash JA, Varghese GM. Severe scrub typhus infection: Clinical features, diagnostic challenges and management. World J Crit Care Med 2015; 4: 244-50. DOI: https://doi.org/10.5492/wjccm.v4.i3.244
Blanton LS. Murine Typhus: A review of a reemerging flea-borne rickettsiosis with potential for neurologic manifestations and sequalae. Infect Dis Rep 2023; 15: 700-16. DOI: https://doi.org/10.3390/idr15060063
Thap LC, Supanaranond W, Treeprasertsuk S, Kitvatanachai S, Chinprasatsak S, Phonrat B. Septic shock secondary to scrub typhus: characteristics and complications. Southeast Asian J Trop Med Public Health 2002; 33: 780-6.
Tran HTD, Schindler C, Pham TTT, Vien MQ, Do HM, Ngo QT, et al. Simple clinical and laboratory predictors to improve empirical treatment strategies in areas of high scrub typhus and dengue endemicity, central Vietnam. PLoS Negl Trop Dis 2022; 16: e0010281. DOI: https://doi.org/10.1371/journal.pntd.0010281
Prakash JAJ. Scrub typhus: risks, diagnostic issues, and management challenges. Res Rep Trop Med 2017; 8: 73-83. DOI: https://doi.org/10.2147/RRTM.S105602
Stewart AG, Stewart AGA. An Update on the laboratory diagnosis of Rickettsia spp. Infection. Pathogens 2021; 10: 1319. DOI: https://doi.org/10.3390/pathogens10101319
Harris PNA, Oltvolgyi C, Islam A, HussainYusuf H, Loewenthal MR, Vincent G, et al. An outbreak of scrub typhus in military personnel despite protocols for antibiotic prophylaxis: doxycycline resistance excluded by a quantitative PCR-based susceptibility assay. Microbes Infect 2016; 18: 406-11. DOI: https://doi.org/10.1016/j.micinf.2016.03.006
Balasubramanian P, Sharma N, Biswal M, Bhalla A, Kumar S, Kumar V. Critical illness scoring systems: sequential organ failure assessment, acute physiology and chronic health evaluation II, and quick sequential organ failure assessment to predict the clinical outcomes in scrub typhus patients with organ dysfunctions. Indian J Crit Care Med 2018; 22: 706-10. DOI: https://doi.org/10.4103/ijccm.IJCCM_254_18
Guan XG, Wei YH, Jiang BG, Zhou SX, Zhang AR, Lu QB, et al. Clinical characteristics and risk factors for severe scrub typhus in pediatric and elderly patients. PLoS Negl Trop Dis 2022; 16: e0010357. DOI: https://doi.org/10.1371/journal.pntd.0010357
Kim MH, Kim SH, Choi JH, Wie SH. Clinical and laboratory predictors associated with complicated scrub typhus. Infect Chemother 2019; 51: 161-70. DOI: https://doi.org/10.3947/ic.2019.51.2.161
Kim DM, Kim SW, Choi SH, Yun NR. Clinical and laboratory findings associated with severe scrub typhus. BMC Infect Dis 2010; 10: 108. DOI: https://doi.org/10.1186/1471-2334-10-108
Bonell A, Lubell Y, Newton PN, Crump JA, Paris DH. Estimating the burden of scrub typhus: A systematic review. PLoS Negl Trop Dis 2017; 11(9): e0005838. DOI: https://doi.org/10.1371/journal.pntd.0005838
Thipmontree W, Tantibhedhyangkul W, Silpasakorn S, Wongsawat E, Waywa D, Suputtamongkol Y. Scrub typhus in northeastern Thailand: eschar distribution, abnormal electrocardiographic findings, and predictors of fatal outcome. Am J Trop Med Hyg 2016; 95: 769-73. DOI: https://doi.org/10.4269/ajtmh.16-0088
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







