EFFICACY OF LACTOSE-FREE FORMULA AS A 24-HOUR MANAGEMENT APPROACH FOR ACUTE DIARRHEA AMONG CHILDREN
DOI:
https://doi.org/10.55374/jseamed.v7.175Keywords:
Acute diarrhea, Lactose intolerance, Lactose-free formulaAbstract
Background: Diarrhea continues to be a prominent contributor to morbidity and mortality among young children under five years, especially in developing nations. Secondary lactose intolerance is a significant complication that can arise from acute diarrhea. However, it can be effectively managed with lactose-free formula.
Objective: This study aimed to compare the rate of diarrhea resolution within a 24-hour period among children receiving lactose-free formula and those receiving lactose-containing formula.
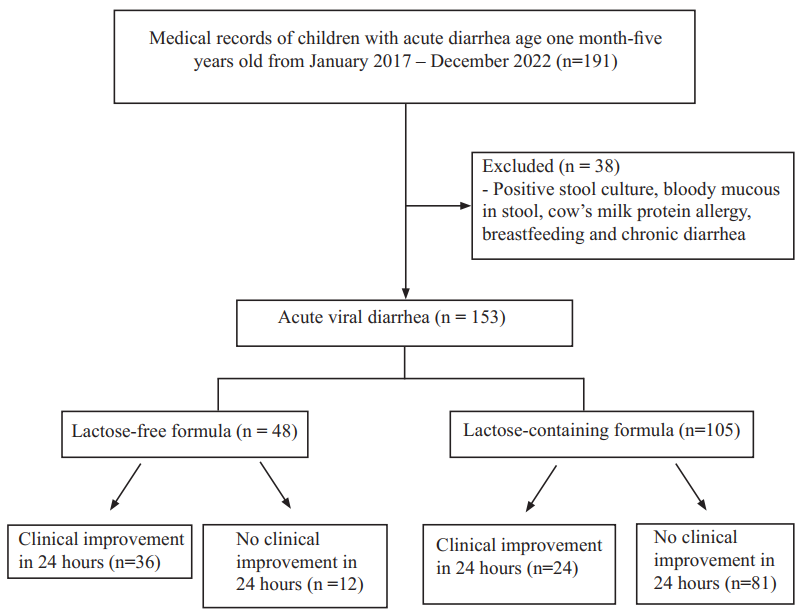
Methods: This retrospective cohort study took place at Naresuan University Hospital and included 153 children aged between one month and five years admitted with acute diarrhea. Participants with bloody mucous diarrhea suspected to be bacterial in nature, positive stool culture, breastfeeding and chronic diarrhea (including cow’s milk protein allergy and inflammatory bowel disease) were excluded. We compared the effectiveness of lactose-free formula (n=48) and lactose-containing formula in improving clinical diarrhea within a 24-hour (n=105).
Results: The study findings indicated the lactose-free formula group demonstrated a statistically significant increase in efficacy, with a 3.90 fold improvement in diarrhea within 24 hours compared with that of the group receiving lactose-containing formula. These results were obtained after the confounding factors were adjusted using multivariable regression analysis. The adjusted relative risk (RR) for a 24-hour improvement in diarrhea was 3.90 (95% CI: 1.91-7.95). However, this study encountered limitations regarding the sample size and accurate measurement of stool output.
Conclusion: Lactose-free formula showed the potential for greater effectiveness in improving acute diarrhea within a 24-hour timeframe compared with lactose-containing formula.
Downloads
Metrics
References
Farthing M, Salam MA, Lindberg G, Dite P, Khalif I, Salazar-Lindo E., et al. Acute diarrhea in adults and children: a global perspective. J Clin Gastroenterol 2013; 47: 12-20. DOI: https://doi.org/10.1097/MCG.0b013e31826df662
The Thai Society of Pediatric Gastroenterology and Hepatology. Clinical practice guideline for acute diarrhea in children. 2562. [cited 2021 November 27]. Available from: http://www.pthaigastro.org/Document/hz0tpx1bdldozf11z5minfimCPG_Blue.pdf
Department of Disease Control. Diarrhea situation in Thailand at 9 November 2019. [cited 2021 November 27]. Available from: https://ddc.moph.go.th/uploads/files/a38f-502166f15054034c545848278ac8.pdf
Saunders N, Friedman JN. Lactose avoidance for young children with acute diarrhea Paediatr Child Health 2014; 19: 529-30. DOI: https://doi.org/10.1093/pch/19.10.529
Raithel M, Weidenhiller M, Hagel AF, Hetterich U, Neurath MF, Konturek PC. The malabsorption of commonly occurring mono and disaccharides: levels of investigation and differential diagnoses. Dtsch Arztebl Int 2013; 110: 775-782. DOI: https://doi.org/10.3238/arztebl.2013.0775
Heyman MB. Committee on Nutrition. Lactose intolerance in infants, children, and adolescents. Pediatrics 2006; 118: 1279-86. DOI: https://doi.org/10.1542/peds.2006-1721
Guarino A, Ashkenazi S, Gendrel D, Lo Vecchio A, Shamir R, Szajewska H. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases. Evidence Based Guidelines for the Management of Acute Gastroenteritis in Children in Europe: Update 2014. J Pediatr Gastroenterol Nutr 2014; 59: 132-52. DOI: https://doi.org/10.1097/MPG.0000000000000375
Ngeonmak T. Efficacy of adjunctive treatment in acute diarrhea. Thai J Pediatr 2562; 58: 113-20.
Simakachorn N, Tongpenyai Y, Tongtan O, Varavithya W. Randomized, double-blind clinical trial of a lactose-free and a lactosecontaining formula in dietary management of acute childhood diarrhea. J Med Assoc Thai 2004; 87: 641-49.
Hartawan IN, Soenarto S, Suandi IKG. Effectiveness of lactose-free formula in management of acute rotavirus diarrhea. Paediatr Indones 2009; 49: 299-303. DOI: https://doi.org/10.14238/pi49.5.2009.299-303
MacGillivray S, Fahey T, McGuire W. Lactose avoidance for young children with acute diarrhoea. Cochrane Database Syst Rev. 2013; 2013 (10): CD005433. DOI: https://doi.org/10.1002/14651858.CD005433.pub2
Soeparto P, Stobo EA, Walker-Smith JA. Role of chemical examination of the stool in diagnosis of sugar malabsorption in children. Arch Dis Child 1972; 47: 56-61. DOI: https://doi.org/10.1136/adc.47.251.56
Erickson JA, Case K, Neider C, Johnson LM. Stool Reducing Sugars and Stool pH Are Poor Screening Tests for Intestinal Disaccharidase Deficiencies in Children. J Appl Lab Med 2020; 5: 257-62. DOI: https://doi.org/10.1093/jalm/jfz017
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







