IMPACT OF THE COVID-19 PANDEMIC ON FRAGILITY HIP FRACTURE MANAGEMENT AND MORTALITY RATE
DOI:
https://doi.org/10.55374/jseamed.v7.155Keywords:
COVID-19, Fragility hip fracture, Osteoporotic fracture, MortalityAbstract
Background: The COVID-19 pandemic has greatly affected patients without COVID, including osteoporotic hip fractures. Treatment protocols and time for surgery have been disrupted and delayed resulting in unsatisfactory outcomes. This study compared the mortality rate among patients with osteoporotic hip fractures during the COVID-19 pandemic and during the prepandemic periods.
Methods: The patients’ information recorded in the Fracture Liaison Service (FLS) registry was retrospectively reviewed. We defined the prepandemic group as the admissions between May 2019 and March 2020 and the pandemic group as admissions from April 2020 to February 2021. The demographic data were collected, including serum calcium and 25(OH)D levels. Time to surgery, postoperative complications, length of stay and death were obtained and compared between the two periods.
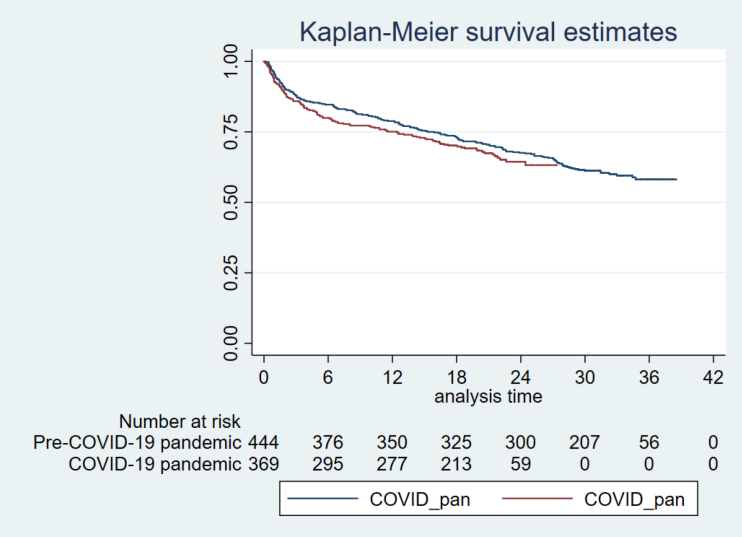
Results: We included 813 patients, with 444 and 369 patients in the prepandemic and the pandemic groups, respectively. Mean age, sex and comorbidities were comparable in both groups. The proportion of patients with insufficient and deficient vitamin D was significantly higher in the pandemic group (46.41 vs. 62.85%, p<0.01). Time to surgery and length of hospital stay was significantly longer in the pandemic period (p <0.05). The mortality was higher but did not significantly differ in the pandemic period with an adjusted hazard ratio of 1.08 (95% CI = 0.76-1.54).
Conclusion: Properly managing hip fractures during the pandemic is crucial to prevent and reduce morbidity and mortality. Inadequate serum vitamin D level has been noted in the pandemic group but was not associated with mortality rate.
Downloads
Metrics
References
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A. The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 2001; 12: 417-27. DOI: https://doi.org/10.1007/s001980170112
Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int 2005; 16 (Suppl 2): S3-7. DOI: https://doi.org/10.1007/s00198-004-1702-6
Matzkin EG, DeMaio M, Charles JF, Franklin CC. Diagnosis and Treatment of Osteoporosis: What Orthopaedic Surgeons Need to Know. J Am Acad Orthop Surg 2019; 27: e902-e12. DOI: https://doi.org/10.5435/JAAOS-D-18-00600
Daraphongsataporn N, Saloa S, Sriruanthong K, Philawuth N, Waiwattana K, Chonyuen P, et al. One-year mortality rate after fragility hip fractures and associated risk in Nan, Thailand. Osteoporos Sarcopenia 2020; 6: 65-70. DOI: https://doi.org/10.1016/j.afos.2020.05.005
Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 2010; 182: 1609-16. DOI: https://doi.org/10.1503/cmaj.092220
WHO Director-General’s opening remarks at the media briefing on COVID-19 -March 2020.https://www.youtube.com/watch?v=sbT6AANFOm4
Crozier-Shaw G, Hughes AJ, Conlon B, Sheehan E, Merghani K. Hip fracture care during Covid-19: a regional trauma centre’s experience. Ir J Med Sci 2021; 190: 1275-80. DOI: https://doi.org/10.1007/s11845-020-02476-0
Kongtush C, Supphamard L, Urawit P. Mortality and Prognosis Factors of Elderly Patients with Pertrochanteric Fracture: Re-evaluation in Maharat Nakhon Ratchasima Hospital. Thai J Ortho Surg 2015; 39: 3-9.
Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth 2008; 55: 146-54. DOI: https://doi.org/10.1007/BF03016088
Zhu Y, Chen W, Xin X, Yin Y, Hu J, Lv H, et al. Epidemiologic characteristics of traumatic fractures in elderly patients during the outbreak of coronavirus disease 2019 in China. Int Ortho 2020; 44: 1565-70. DOI: https://doi.org/10.1007/s00264-020-04575-0
Kılıç B, Gülabi D, Agar A, Büyükdoğan H, Şahin A, Eren E, et al. How did restrictions mandated by the COVID-19 pandemic affect the performance of orthopedic trauma surgery in a Level-1 tertiary trauma hospital? Ulus Travma Acil Cerrahi Derg 2021; 27: 547-51.
Sephton BM, Mahapatra P, Shenouda M, Ferran N, Deierl K, Sinnett T, et al. The effect of COVID-19 on a Major Trauma Network. An analysis of mechanism of injury pattern, referral load and operative case-mix. Injury 2021; 52: 395-401. DOI: https://doi.org/10.1016/j.injury.2021.02.035
Nuñez JH, Sallent A, Lakhani K, GuerraFarfan E, Vidal N, Ekhtiari S, et al. Impact of the COVID-19 Pandemic on an Emergency Traumatology Service: Experience at a Tertiary Trauma Centre in Spain. Injury 2020; 51: 1414-8. DOI: https://doi.org/10.1016/j.injury.2020.05.016
Anusitviwat C, Vanitcharoenkul E, Chotiyarnwong P, Unnanuntana A. Surgical treatment for fragility hip fractures during the COVID-19 pandemic resulted in lower short-term postoperative functional outcome and a higher complication rate compared to the pre-pandemic period. Osteoporos Int 2022; 33: 2217-26. DOI: https://doi.org/10.1007/s00198-022-06485-w
Jarvis S, Salottolo K, Madayag R, Pekarek J, Nwafo N, Wessel A, et al. Delayed hospital admission for traumatic hip fractures during the COVID-19 pandemic. J Orthop Surg Res 2021; 16: 237. DOI: https://doi.org/10.1186/s13018-021-02382-w
Narang A, Chan G, Aframian A, Ali Z, Carr A, Goodier H, et al. Thirty-day mortality following surgical management of hip fractures during the COVID-19 pandemic: findings from a prospective multi-centre UK study. Int Orthop 2021; 45: 23-31. DOI: https://doi.org/10.1007/s00264-020-04739-y
Wang N, Chen Y, Ji J, Chang J, Yu S, Yu B. The relationship between serum vitamin D and fracture risk in the elderly: a meta-analysis. J Orthop Surg Res 2020; 15: 81. DOI: https://doi.org/10.1186/s13018-020-01603-y
Feng Y, Cheng G, Wang H, Chen B. The associations between serum 25-hydroxyvitamin D level and the risk of total fracture and hip fracture. Osteoporos Int 2017; 28: 1641-52. DOI: https://doi.org/10.1007/s00198-017-3955-x
Weaver CM, Alexander DD, Boushey CJ, Dawson-Hughes B, Lappe JM, LeBoff MS, et al. Calcium plus vitamin D supplementation and risk of fractures: an updated metaanalysis from the National Osteoporosis Foundation. Osteoporos Int 2016; 27: 367-76. DOI: https://doi.org/10.1007/s00198-015-3386-5
Torres-Naranjo F, De la Peña-Rodríguez P, López-Cervantes RE, Morales-Torres J, Morales-Vargas J, Gutiérrez-Hermosillo H, et al. Joint position statement on management of patient with osteoporosis during COVID-19 contingency from the AMMOM, CONAMEGER, FELAEN, FEMECOG, FEMECOT, and ICAAFYD. Arch Osteoporos 2021; 16:18. DOI: https://doi.org/10.1007/s11657-020-00869-3
Hampson G, Stone M, Lindsay JR, Crowley RK, Ralston SH. Diagnosis and Management of Osteoporosis During COVID-19: Systematic Review and Practical Guidance. Calcif Tissue Int 2021; 109: 351-62. DOI: https://doi.org/10.1007/s00223-021-00858-9
McCloskey EV, Harvey NC, Johansson H, Lorentzon M, Vandenput L, Liu E, et al. Global impact of COVID-19 on non-communicable disease management:descriptive analysis of access to FRAX fracture risk online tool for prevention of osteoporotic fractures. Osteoporos Int 2021; 32: 39-46. DOI: https://doi.org/10.1007/s00198-020-05542-6
Stephens A, Rudd H, Stephens E, Ward J. Secondary Prevention of Hip Fragility Fractures During the COVID-19 Pandemic: Service Evaluation of “MRS BAD BONES”. JMIR Aging 2020; 3: e25607. DOI: https://doi.org/10.2196/25607
Falchetti A, Mohseni M, Tramontana F, Napoli N. Secondary prevention of fragility fractures: where do we stand during the COVID-19 pandemic? J Endocrinol Invest 2021; 44: 2521-4. DOI: https://doi.org/10.1007/s40618-021-01552-1
Napoli N, Elderkin AL, Kiel DP, Khosla S. Managing fragility fractures during the COVID-19 pandemic. Nat Rev Endocrinol 2020; 16: 467-8. DOI: https://doi.org/10.1038/s41574-020-0379-z
Kong SH, Hwang BK, Yoon BH. The Impact of COVID-19 on the Optimal Management of Osteoporosis. J Bone Metab 2021; 28: 115-22. DOI: https://doi.org/10.11005/jbm.2021.28.2.115
Tarantino U, Cariati I, Tancredi V, Casamassima D, Piccirilli E, Iundusi R, et al. State of Fragility Fractures Management during the COVID-19 Pandemic. Int J Environ Res Public Health 2020; 17: 7732 DOI: https://doi.org/10.3390/ijerph17217732
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







