PREVALENCE AND FACTORS ASSOCIATED WITH FOREIGN BODY ASSOCIATED OCULAR INJURY AMONG OCULAR INJURY PATIENTS IN FOUR COMMUNITY HOSPITALS, CENTRAL, THAILAND: A MULTICENTER STUDY
DOI:
https://doi.org/10.55374/jseamed.v9.233Keywords:
foreign body-associated ocular injury, ocular injury, factor association, community hospitalAbstract
Background: Foreign body (FB) associated ocular injury is a common cause of eye trauma. Understanding the prevalence and associated factors of FB-associated ocular injuries is essential for developing targeted prevention strategies and improving healthcare access for ocular trauma in community areas.
Objectives: This study aimed to determine the prevalence and associated factors of FB-associated ocular injuries among patients presenting with ocular trauma at four community hospitals in central Thailand.
Methods: This cross-sectional multicenter study reviewed ocular injury cases in four community hospitals in central Thailand, identified by ICD-10 codes from October 1, 2018, to September 17, 2024. Characteristics of FB-associated ocular injury, defined as ocular trauma with history or examination indicating a foreign body as the causative agent, were reviewed from medical records. Descriptive statistics and chi-square tests were used to analyze the differences between groups. Prevalence ratios (PRs) with 95% confidence intervals (CIs) were estimated using Poisson regression with robust variance to assess associations. Temporal trends were examined by fiscal year periods.
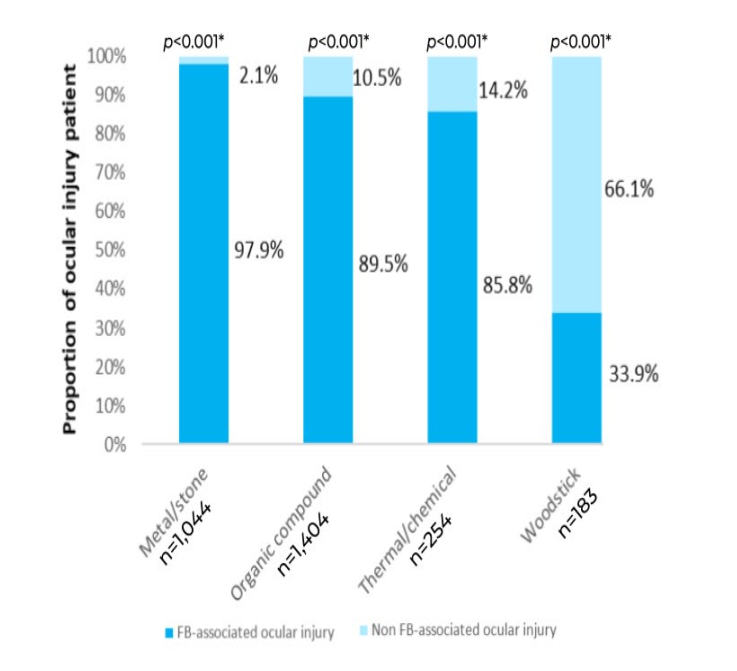
Results: Of 7,189 participants (60.8% male; mean age 45 years), 62% (n=4,456) had FB-associated ocular injuries. Male gender (aPR 1.12, 95% CI 1.08–1.16), metal/stone objects (aPR 1.53, 95% CI 1.46–1.59), and injury onset ≥24 hours (aPR 1.24, 95% CI 1.17–1.32) were associated with a higher risk. Trend analysis by fiscal year showed that health-seeking behavior shifted toward OPD visits (p<0.001).
Conclusion: The prevalence of FB-associated ocular injuries in community hospitals was high, with male gender, mechanical work, metallic objects, and delayed healthcare access (>24 hours) identified as significant risk factors. Preventive strategies such as promoting protective measures in industrial sectors and emphasizing the importance of seeking timely healthcare are essential to reducing the injury burden. Since 2019, a shift in healthcare access from ER to OPD has been observed, underscoring the need for a flexible healthcare system that can adapt to changing health-seeking behaviors.
Downloads
Metrics
References
Schein OD, Hibberd PL, Shingleton BJ, Kunzweiler T, Fambach DA, Seddon JM, et al. The Spectrum and Burden of Ocular Injury. Ophthalmol 1988; 95: 300-5. DOI: https://doi.org/10.1016/S0161-6420(88)33183-0
Sanchez MAT, Parulan MAA. Association of demographic characteristics and behavioral risk with the type and severity of injury of ocular trauma among patients presenting in a provincial level III government hospital: A 5-year analytic cross-sectional study. Int J Ophthalmol Clin Res 2022; 9:145. DOI: https://doi.org/10.23937/2378-346X/1410145
Li C, Fu Y, Liu S, Yu H, Yang X, Zhang M, et al. The global incidence and disability of eye injury: an analysis from the global burden of disease study 2019. E Clin Med 2023; 62: 102134. DOI: https://doi.org/10.1016/j.eclinm.2023.102134
Al-Attas AH, Williams CD, Pitchforth EL, O’Callaghan CO, Lewallen S. Understanding delay in accessing specialist emergency eye care in a developing country: eye trauma in Tanzania. Ophthalmic Epidemiol 2010; 17: 103-12. DOI: https://doi.org/10.3109/09286580903453522
Loon SC, Tay WT, Saw SM, Wang JJ, Wong TY. Prevalence and risk factors of ocular trauma in an urban Southeast Asian population: the Singapore Malay Eye Study. Clin Exp Ophthalmol 2009; 37: 362-7. DOI: https://doi.org/10.1111/j.1442-9071.2009.02035.x
Haring RS, Canner JK, Haider AH, Schneider EB. Ocular injury in the United States: Emergency department visits from 2006– 2011. Injury 2016; 47: 104-8. DOI: https://doi.org/10.1016/j.injury.2015.07.020
Gupta A, Tripathy K. Intraocular foreign body StatPearls Publishing; 2023.
Cillino S, Casuccio A, Di Pace F, Pillitteri F, Cillino G. A five-year retrospective study of the epidemiological characteristics and visual outcomes of patients hospitalized for ocular trauma in a Mediterranean area. BMC Ophthalmol 2008; 8: 6. DOI: https://doi.org/10.1186/1471-2415-8-6
Wang W, Zhou Y, Zeng J, Shi M, Chen B. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in South‐Central China. Acta Ophthalmol 2017; 95. DOI: https://doi.org/10.1111/aos.13438
Imsuwan I, Amnuaypattanapon K, Vongkittirux S, Imsuwan Y. The study of incidence and characteristics of patients with eye-related chief complaints at the Emergency Department of Thammasat University Hospital. Emerg Med Int 2020; 2020: 1-9. DOI: https://doi.org/10.1155/2020/4280543
Tan MM, Driscoll PA, Marsden JE. Management of eye emergencies in the accident and emergency department by senior house officers: a national survey. Emerg Med J 1997; 14: 157-8. DOI: https://doi.org/10.1136/emj.14.3.157
Rehan SM, Morris DS, Pedlar L, Sheen N, Shirodkar A. Ophthalmic emergencies presenting to the emergency department at the University Hospital of Wales, Cardiff, UK. Clin Exp Optom 2020; 103: 895-901. DOI: https://doi.org/10.1111/cxo.13050
Safari S, McLaughlin CJ, Shah A, Kane BG. Prolonged ocular foreign body found on repeat visit to a second emergency department. Cureus 19, 2023; 19; 15: e37819. DOI: https://doi.org/10.7759/cureus.37819
Janda S, Sansuk J. Factors associated with re-attendance at emergency departments among older adults: A cross-sectional analytical study. Inquiry 2025; 62:469580251349652. DOI: https://doi.org/10.1177/00469580251349652
Mahjoub H, Ssekasanvu J, Yonekawa Y, Justin GA, Cavuoto KM, Lorch A, Most common ophthalmic diagnoses in eye Emergency Departments: A multicenter study. Am J Ophthalmol 2023; 254: 36-43. DOI: https://doi.org/10.1016/j.ajo.2023.03.016
Dua HS, Ting DSJ, Al Saadi A, Said DG. Chemical eye injury: pathophysiology, assessment and management. Eye 2020; 34: 2001-19. DOI: https://doi.org/10.1038/s41433-020-1026-6
Shah M, Shah S, Vora S, Batra D, Pandya R. Wooden sticks as objects of ocular injury: Are they really bad? Sudanese J Ophthalmol 2013; 5: 62. DOI: https://doi.org/10.4103/1858-540X.124827
Galvagno SM, Nahmias JT, Young DA. Advanced trauma life support® Update 2019. Anesthesiol Clin 2019; 37: 13-32. 19. Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 2003; 3: 21. DOI: https://doi.org/10.1186/1471-2288-3-21
Austin PC, White IR, Lee DS, van Buuren S. Missing data in clinical research: A tutorial on multiple imputation. Can J Cardiol 2021; 37: 1322-31. DOI: https://doi.org/10.1016/j.cjca.2020.11.010
Wulff J, Ejlskov L. Multiple imputation by chained equations in praxis: guidelines and review. Electron J Bus Res Methods 2017;15: 2017-58.
Haring RS, Canner JK, Haider AH, Schneider EB. Ocular injury in the United States: Emergency department visits from 2006– 2011. Injury 2016; 47: 104-8. DOI: https://doi.org/10.1016/j.injury.2015.07.020
Park J, Yang SC, Choi H young. Epidemiology and clinical patterns of ocular trauma at a level 1 trauma center in Korea. J Korean Med Sci 2021; 36. DOI: https://doi.org/10.3346/jkms.2021.36.e5
Kousiouris P, Gouliopoulos N, Kourtesa A, et al. The demographic and social characteristics of patients with ocular foreign bodies in a Greek Tertiary Hospital. Clin Ophthalmol 2022; 16: 2323-28. DOI: https://doi.org/10.2147/OPTH.S370188
Imsuwan I, Amnuaypattanapon K, Vongkittirux S, Imsuwan Y. The study of incidence and characteristics of patients with eyerelated chief complaints at the Emergency Department of Thammasat University Hospital.
Cillino S, Casuccio A, Di Pace F, Pillitteri F, Cillino G. A five-year retrospective study of the epidemiological characteristics and visual outcomes of patients hospitalized for ocular trauma in a Mediterranean area. BMC Ophthalmol 2008; 8:6. DOI: https://doi.org/10.1186/1471-2415-8-6
Wang W, Zhou Y, Zeng J, Shi M, Chen B. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in South‐Central China. Acta Ophthalmol 2017; 95. DOI: https://doi.org/10.1111/aos.13438
Chatterjee S, Agrawal D. Primary prevention of ocular injury in agricultural workers with safety eyewear. Indian J Ophthalmol 2017; 65: 859. DOI: https://doi.org/10.4103/ijo.IJO_334_17
Turbert D. Safety glasses and protective eyewear prevent potentially blinding eye injuries. American Academy of Ophthalmology, 2023
Mahan M. Ocular Trauma Prevention Strategies and Patient Counseling, 2024.
AlMahmoud T, Elkonaisi I, Grivna M, Abu-Zidan FM. Personal protective eyewear usage among industrial workers in smallscale enterprises. Inj Epidemiol 2020; 7: 54. DOI: https://doi.org/10.1186/s40621-020-00280-z
Choovuthayakorn J, Worakriangkrai V, Patikulsila D, Watanachai N, Kunavisarat P, Chaikitmongkol V, et al. Epidemiology of eye injuries resulting in hospitalization, a referral hospital-based study. Clin Ophthalmol 2020; 14: 1-6. DOI: https://doi.org/10.2147/OPTH.S234035
Chaikitmongkol V, Leeungurasatien T, Sengupta S. Work-related eye injuries. Asia-Pac J Ophthalmol 2015; 4: 155-60. DOI: https://doi.org/10.1097/APO.0000000000000046
şentürk fevzi. Standardized classification of mechanical ocular injuries, efficacy, and shortfalls. Beyoglu Eye Journal. Published online 2021. DOI: https://doi.org/10.14744/bej.2021.01488
Mohseni M, Blair K, Gurnani B, N. Bragg. B. Blunt Eye Trauma StatPearls Publishing, 2023.
Mishra A, Verma AK. Sports related ocular injuries. Med J Armed Forces India 2012; 68: 260-6. DOI: https://doi.org/10.1016/j.mjafi.2011.12.004
Mengistu HG, Alemu DS, Alimaw YA, Yibekal BT. Prevalence of occupational ocular Injury and associated factors among smallscale industry workers in Gondar Town, Northwest Ethiopia, 2019. Clin Optom (Auckl) 2021; 13: 167-74. DOI: https://doi.org/10.2147/OPTO.S290257
Walsh A, Lewis K. EMS Management of Eye Injuries StatPearls Publishing; 2023.
Khatry SK. The epidemiology of ocular trauma in rural Nepal. Brit J Ophthalmol 2004; 88: 456-60. DOI: https://doi.org/10.1136/bjo.2003.030700
K Abu E, Ocansey S, A Gyamfi J, Ntodie M, KA Morny E. Epidemiology and visual outcomes of ocular injuries in a low resource country. Afr Health Sci 2020; 20: 779-88. DOI: https://doi.org/10.4314/ahs.v20i2.31
Jung HC, Lee SY, Yoon CK, Park UC, Heo JW, Lee EK. Intraocular foreign body: diagnostic protocols and treatment strategies in ocular trauma patients. J Clin Med 2021; 10: 1861. DOI: https://doi.org/10.3390/jcm10091861
Heath Jeffery RC, Dobes J, Chen FK. Eye injuries: understanding ocular trauma. Aust J Gen Pract. 2022; 51: 476-82. DOI: https://doi.org/10.31128/AJGP-03-21-5921
Kraemer MUG, Yang CH, Gutierrez B, Wu CH, Clein B, Pigott DM, et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020; 368: 493-7. DOI: https://doi.org/10.1126/science.abb4218
Chen Y, Cai M, Li Z, Lin X, Wang L. Impacts of the COVID-19 Pandemic on public hospitals of different levels: Six-month evidence from Shanghai, China. Risk Manag Healthc Policy 2021; 14: 3635-51. DOI: https://doi.org/10.2147/RMHP.S314604
Giannouchos T V., Biskupiak J, Moss MJ, Brixner D, Andreyeva E, Ukert B. Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am J Emerg Med 2021; 40: 20-26. DOI: https://doi.org/10.1016/j.ajem.2020.12.009
Mahan M, Purt B. Ocular trauma prevention strategies and patient counseling. StatPearls Publishing; 2025
Rho JY, Dryden SC, Jerkins BM, Fowler BT. Management of eye trauma for the primary care physician. J Am Board Fam Med 2021; 34: 1018-29. DOI: https://doi.org/10.3122/jabfm.2021.05.210121
Bamahfouz A, Bakry SM, Alsharif AM, Alomeri S, Alsharif EF, Zamzami OS, et al. Ocular chemical injuries in Western Saudi Arabia: A study of the public’s level of knowledge and experience. Cureus 2023 15: e07404. DOI: https://doi.org/10.7759/cureus.40724
Dhabaan WA, Almutairi KH, Alzahrani AA, Almatlaq AH, Asiri AAHJ, Alshahrani RSH, et al. Assessing knowledge and practice about eye injuries first aid, with awareness about the importance of early management among general population in Asser Region, 2020. J Family Med Prim Care 2021; 10: 2022-27. DOI: https://doi.org/10.4103/jfmpc.jfmpc_2223_20
Seraj H, Khawandanh S, Fatani A, Saeed A, Alotaibi G, Basheikh A. Population-level investigation of the knowledge of ocular chemical injuries and proper immediate action. BMC Res Notes 2020; 13: 103. DOI: https://doi.org/10.1186/s13104-020-04950-5
Adams JSK, Raju R, Solomon V, et al. Increasing compliance with protective eyewear to reduce ocular injuries in stone-quarry workers in Tamil Nadu, India: A pragmatic, cluster randomised trial of a single education session versus an enhanced education package delivered over six months. Injury 2013; 44: 118-25. DOI: https://doi.org/10.1016/j.injury.2011.10.001
De Silva I, Thomas MG, Shirodkar AL, Kuht HJ, Ku JY, Chaturvedi R, et al. Patterns of attendances to the hospital emergency eye care service: a multicentre study in England. Eye 2022; 36: 2304-11. DOI: https://doi.org/10.1038/s41433-021-01849-8
Mullan B, Smith L, Sainsbury K, Allom V, Paterson H, Lopez AL. Active behaviour change safety interventions in the construction industry: A systematic review. Saf Sci 2015; 79: 139-48. Emerg Med Int 2020; 2020:1-9. DOI: https://doi.org/10.1016/j.ssci.2015.06.004
Downloads
Additional Files
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







