AN ASSOCIATION BETWEEN CARDIO-ANKLE VASCULAR INDEX (CAVI) AND VENTRICULAR-ARTERIAL COUPLING IN THAI CHRONIC KIDNEY DISEASE PATIENTS
DOI:
https://doi.org/10.55374/jseamed.v8.217Keywords:
Chronic kidney disease, heart failure with mildly reduced ejection fraction, heart failure with preserved ejection fraction, cardio-ankle vascular index, ventricular-arterial coupling, mortalityAbstract
Background: Cardiovascular remodeling is a recognized chronic kidney disease (CKD) complication. The clinical implication of heart failure with mildly reduced ejection fraction (HFmrEF) and preserved ejection fraction (HFpEF) in CKD, including their underlying pathogenic mechanisms, remains incompletely understood.
Objectives: This study aimed to determine the association between arterial stiffness, as measured by the cardio-ankle vascular index (CAVI), and impaired interaction between the left ventricle and the arterial system by ventricular-arterial coupling (VAC) determined by echocardiography with heart failure with HFmrEF or HFpEF in non-dialysis CKD. Secondly, to evaluate the prognostic impact of baseline HFmrEF/HFpEF, abnormal CAVI, and VAC on long-term outcomes.
Methods: A cross-sectional and prospective analysis was conducted in the CORE-CKD cohort of 66 non-dialysis CKD patients, stages 3-5. The relationship between CAVI or VAC and HFmrEF/HFpEF at baseline was assessed using multivariate logistic regression. Subsequently, the association between HFmrEF/HFpEF, high CAVI, and high VAC with a composite outcome of all-cause mortality and cardiovascular hospitalization was evaluated using the multivariate Cox proportional hazards model.
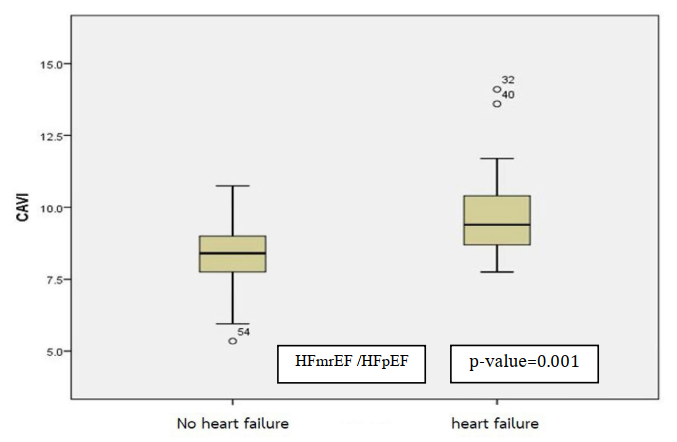
Results: At baseline, those with HFmrEF/HFpEF (n=18) had significantly higher CAVI (9.4 vs. 8.4, p=0.001) and VAC values (1.02 vs. 0.88, p=0.033) than those without HFmrEF/HFpEF. High CAVI was significantly associated with HFmrEF/HFpEF by multivariate analysis (OR 5.11, 95% CI: 1.27-20.42). This prospective study showed that the median follow-up time was six years. The risk for primary composite outcome was substantially higher in patients with HFmrEF/HFpEF than those without (HR 43.8, 95%CI: 5.89-304.8).
Conclusion: HFmrEF/HFpEF was associated with increased arterial stiffness, impaired left ventricular-arterial coupling, and a significantly elevated risk of mortality or cardiovascular hospitalization among CKD patients.
Downloads
Metrics
References
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease – a systematic review and meta-analysis. PLOSONE 2016; 11: e0158765. DOI: https://doi.org/10.1371/journal.pone.0158765
Provenzano M, Coppolino G, Faga T, Garofalo C, Serra R, Andreucci M. Epidemiology of cardiovascular risk in chronic kidney disease patients: the real silent killer. Rev Cardiovasc Med 2019; 20: 209-20. DOI: https://doi.org/10.31083/j.rcm.2019.04.548
Webster AC, Nagler EV, Morton RL, Masson P. Chronic kidney disease. The Lancet 2017; 389: 1238–52. DOI: https://doi.org/10.1016/S0140-6736(16)32064-5
Tonelli M, Karumanchi SA, Thadhani R. Epidemiology and mechanisms of uremia-related cardiovascular disease. Circulation 2016; 133: 518–36. DOI: https://doi.org/10.1161/CIRCULATIONAHA.115.018713
Townsend RR. Arterial stiffness and chronic kidney disease: lessons from the chronic renal insufficiency cohort study. Curr Opin Nephrol Hypertens 2015; 24: 47-53. DOI: https://doi.org/10.1097/MNH.0000000000000086
Vasan RS, Short MI, Niiranen TJ, Xanthakis V, DeCarli C, Cheng S, Seshadri S, Mitchell GF. Interrelations Between Arterial Stiffness, Target Organ Damage, and Cardiovascular Disease Outcomes. J Am Heart Assoc 2019; 8: e012141. DOI: https://doi.org/10.1161/JAHA.119.012141
Namba T, Masaki N, Takase B, Adachi T. Arterial Stiffness Assessed by Cardio-Ankle Vascular Index. Int J Mol Sci 2019; 20: 3664. DOI: https://doi.org/10.3390/ijms20153664
Tavolinejad H, Erten O, Maynard H, Chirinos JA. Prognostic value of cardio-ankle vascular Index for cardiovascular and kidney outcome: systemic review and meta-analysis. JACC: Advances 2024; 3: 101019. DOI: https://doi.org/10.1016/j.jacadv.2024.101019
Marakami K, Inayama E, Itoh Y, Tuchiya S, Iwasaki M, Tamura N, et al. The role of Cardio-ankle vascular index as a predictor of mortality in patients on maintenance Hemodialysis. Vasc Health Risk Manag 2021; 17: 791-8. DOI: https://doi.org/10.2147/VHRM.S339769
Hitsumoto T. Clinical usefulness of the cardio-ankle vascular index as a predictor of primary cardiovascular events in patients with chronic kidney disease. J Clin Med Res 2018; 10: 883-90. DOI: https://doi.org/10.14740/jocmr3631
Aiumtrakul N, Supasyndh O, Krittayaphong R, Phrommintikul A, Satirapoj B. Cardioankle vascular index with renal progression and mortality in high atherosclerosis risk: a prospective cohort study in CORE-Thailand. Clin Exp Nephrol 2022; 26: 247-56. DOI: https://doi.org/10.1007/s10157-021-02149-x
Borlaug BA, Kass DA. Ventricular-vascular interaction in heart failure. Cardiol Clin 2011; 29: 447-59. DOI: https://doi.org/10.1016/j.ccl.2011.06.004
Shim CY, Hong GR, Ha JW. Ventricular stiffness and ventricular-arterial coupling in heart failure: what is it, how to assess, and why?. Heart Fail Clin 2019; 15: 267–74. DOI: https://doi.org/10.1016/j.hfc.2018.12.006
Chirinos JA. Ventricular-arterial coupling: Invasive and non-invasive assessment. Artery Res 2013; 7: 10. DOI: https://doi.org/10.1016/j.artres.2012.12.002
Chirinos JA, Sweitzer N. Ventricular-Arterial Coupling in Chronic Heart Failure. Card Fail Rev 2017; 3: 12-8. DOI: https://doi.org/10.15420/cfr.2017:4:2
Chemla D, Antony I, Lecarpentier Y, Nitenberg A. Contribution of systemic vascular resistance and total arterial compliance to effective arterial elastance in humans. Am J Physiol Heart Circ Physiol 2003; 285: H614-20. DOI: https://doi.org/10.1152/ajpheart.00823.2002
Yokoyama H, Yamanaka F, Shishido K, Ochiai T, Yokota S, Moriyama N, et al. Prognostic value of ventricular-arterial coupling after transcatheter aortic valve replacement on midterm clinical outcomes. J Am Heart Assoc 2021; 10: e019267.
Trambaiolo P, Bertini P, Borrelli N, Poli M, Romano S, Ferraiuolo G, et al. Evaluation of ventriculo-arterial coupling in ST elevation myocardial infarction with left ventricular dysfunction treated with levosimendan. Int J Cardiol 2019; 288: 1-4. DOI: https://doi.org/10.1016/j.ijcard.2019.04.052
Obokata M, Kurosawa K, Ishida H, Ito K, Ogawa T, Ando Y, et al. Incremental prognostic value of ventricular-arterial coupling over ejection fraction in patients with maintenance hemodialysis. J Am Soc Echocardiogr 2017; 30: 444-53. e2. DOI: https://doi.org/10.1016/j.echo.2016.12.014
Narayan H, French B, Khan A, Plappert T, Hyman D, Bajulaiye A, et al. Noninvasive measures of ventricular-arterial coupling and circumferential strain predict cancer therapeutics-related cardiac dysfunction. JACC: Cardiovasc Imaging 2016; 9: 1131-41. DOI: https://doi.org/10.1016/j.jcmg.2015.11.024
Edwards NC, Ferro CJ, Townend JN, Steeds RP. Aortic distensibility and arterial-ventricular coupling in early chronic kidney disease: a pattern resembling heart failure with preserved ejection fraction. Heart 2008; 94: 1038-43. DOI: https://doi.org/10.1136/hrt.2007.137539
Savarese G, Stolfo D, Sinagra G, Lund LH. Heart failure with mid-range or mildly reduced ejection fraction. Nat Rev Cardiol 2022; 19: 100-16. DOI: https://doi.org/10.1038/s41569-021-00605-5
Smith DH, Thorp ML, Gurwitz JH, McManus DD, Goldberg RJ, Allen LA, et al. Chronic kidney disease and outcomes in heart failure with preserved versus reduced ejection fraction: the Cardiovascular Research Network PRESERVE Study. Circ Cardiovasc Qual Outcomes 2013; 6: 333–42. DOI: https://doi.org/10.1161/CIRCOUTCOMES.113.000221
Van Deursen VM, Urso R, Laroche C, Damman K, Dahlström U, Tavazzi L, et al. Comorbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail 2014; 16: 103–11. DOI: https://doi.org/10.1002/ejhf.30
Chen C, Liu Y, Xu Y, Xu D. Association between arterial stiffness and heart failure with preserved ejection fraction. Front Cardiovasc Med. 2021; 8: 707162. DOI: https://doi.org/10.3389/fcvm.2021.707162
Sagi B, Keso I, Vas T, Csiky B, Nagy J, Kovacs T. Relationship between arterial stiffness, left ventricular diastolic function, and renal function in chronic kidney disease. BMC Nephrol 2023; 24: 261. DOI: https://doi.org/10.1186/s12882-023-03308-w
Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis 2014; 63: 713-35. DOI: https://doi.org/10.1053/j.ajkd.2014.01.416
Eknoyan G, Lameire N, Eckardt K, Kasiske B, Wheeler D, Levin A et, al. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney int 2013; 3: 5-14.
Bozkurt B, Coats AJS, Tsutsui H, Abdelhamid CM, Adamopoulos S, Albert N, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. Eur J Heart Fail 2021; 23: 352-80. DOI: https://doi.org/10.1002/ejhf.2115
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022; 145: e895-e1032. DOI: https://doi.org/10.1161/CIR.0000000000001073
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021; 42: 3599-726. DOI: https://doi.org/10.1093/eurheartj/ehab368
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens 2023; 41: 1874-2071. DOI: https://doi.org/10.1097/HJH.0000000000003480
Petersmann A, Müller-Wieland D, Müller UA, Landgraf R, Nauck M, Freckmann G, et al. Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes 2019; 127: S1-S7. DOI: https://doi.org/10.1055/a-1018-9078
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015; 28: 1-39.e14. DOI: https://doi.org/10.1016/j.echo.2014.10.003
Chen CH, Fetics B, Nevo E, Rochitte CE, Chiou KR, Ding PA, Kawaguchi M, Kass DA. Noninvasive single-beat determination of left ventricular end-systolic elastance in humans. J Am Coll Cardiol 2001; 38: 2028-34. DOI: https://doi.org/10.1016/S0735-1097(01)01651-5
Burkhoff D, Mirsky I, Suga H. Assessment of systolic and diastolic ventricular properties via pressure-volume analysis: a guide for clinical, translational, and basic researchers. Am J Physiol Heart Circ Physiol 2005; 289: H501-12. DOI: https://doi.org/10.1152/ajpheart.00138.2005
Antonini-Canterin F, Poli S, Vriz O, Pavan D, Bello VD, Nicolosi GL. The VentricularArterial Coupling: From Basic Pathophysiology to Clinical Application in the Echocardiography Laboratory. J Cardiovasc Echogr 2013; 23: 91–5. DOI: https://doi.org/10.4103/2211-4122.127408
Patel RN, Sharma A, Prasad A, Bansal S. Heart failure with preserved ejection fraction with CKD: a narrative review of a multispecialty disorder. Kidney Med 2023; 5: 100705. DOI: https://doi.org/10.1016/j.xkme.2023.100705
Tsao CW, Lyass A, Enserro D, Larson MG, Ho JE, Kizer JR, et al. Temporal trends in the incidence of and mortality associated with heart failure with preserved and reduced ejection fraction. JACC Heart Fail 2018; 6:678-85. DOI: https://doi.org/10.1016/j.jchf.2018.03.006
Zelnick LR, Shlipak MG, Soliman EZ, Anderson A, Christenson R, Kansal M, et al. Prediction of Incident Heart Failure in CKD: the CRIC study. Kidney Int Rep 2022; 7: 708-19. DOI: https://doi.org/10.1016/j.ekir.2022.01.1067
Schupp T, Weidner K, Lau F, Forner J, Schmitt A, Reinhardt M, et, al. Effect of severity and etiology of chronic kidney disease in patients with heart failure with mildly reduced ejection fraction. Clin Res Cardiol 2024: 1-11. DOI: https://doi.org/10.1007/s00392-024-02453-y
Zanoli L, Lentini P, Briet M, Castellino P, House AA, London GM, et al. Arterial stiffness in the heart disease of CKD. J Am Soc Nephrol 2019; 30: 918-28. DOI: https://doi.org/10.1681/ASN.2019020117
Zuo M, Chen Q, PU L, Shi L. Impact of hemodialysis on left ventricular-arterial coupling in end-stage renal disease patients. Blood Purification 2023; 52: 702-11. DOI: https://doi.org/10.1159/000531188
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.







